Understanding Q Fever: The Forgotten Zoonotic Infection
Q fever, a zoonotic disease caused by the bacterium Coxiella burnetii, is often overlooked despite its global prevalence and potential for significant health impacts. Described as a “neglected zoonosis” by the World Health Organization (WHO), Q fever affects both humans and animals, with serious implications for public health, particularly in regions with close human-animal interactions.
What Is Q Fever?
Q fever, sometimes called “query fever” due to its mysterious origins when first identified in 1935 among abattoir workers in Queensland, Australia, is a bacterial infection caused by Coxiella burnetii. This gram-negative, intracellular bacterium is highly resilient, surviving harsh environmental conditions like heat, drying, and disinfectants, making it a persistent threat. Unlike many pathogens, C. burnetii can spread through aerosolized particles, requiring as few as 1–10 organisms to cause infection, which classifies it as a potential bioterrorism agent by the CDC.
Q fever is zoonotic, meaning it spreads from animals to humans, primarily through inhalation of contaminated dust from animal waste, birth products (e.g., placenta, amniotic fluid), urine, feces, or milk. While it rarely causes symptoms in animals, it can lead to reproductive issues like miscarriages in livestock. In humans, Q fever manifests as acute or chronic illness, with symptoms ranging from mild flu-like complaints to life-threatening complications like endocarditis. Its underdiagnosis, due to nonspecific symptoms and limited surveillance in many regions, earns it the title of a “forgotten” zoonotic infection.
Causes and Transmission of Q Fever
1. Primary Reservoirs and Transmission
C. burnetii is found worldwide, except in New Zealand and Antarctica, and infects a wide range of hosts, including cattle, sheep, goats, and occasionally pets like dogs and cats. The bacterium is primarily transmitted to humans through:
- Inhalation of Contaminated Dust: Aerosolized particles from infected animal waste or birthing products are the most common transmission route. You most commonly get it from inhaling dust contaminated by bodily fluids of infected animals.
- Contact with Animal Products: Handling contaminated milk, wool, or meat can spread the bacteria, though ingestion (e.g., unpasteurized milk) is less common.
- Tick-Borne Transmission: Rarely, ticks can transmit C. burnetii to humans or between animals.
- Occupational Exposure: Farmers, veterinarians, abattoir workers, and laboratory personnel working with infected animals are at higher risk. The CDC highlights, “People with certain jobs are at increased risk for exposure to Coxiella burnetii, including veterinarians, meat processing plant workers, dairy workers, livestock ranchers, and researchers.”
Psoriasis: Causes, Symptoms, Diagnosis, and Treatment
2. Environmental Persistence
C. burnetii’s ability to survive in soil and dust for months, even in extreme conditions, contributes to its spread. Outbreaks have been linked to livestock farming, particularly during birthing seasons when bacterial loads are high. For example, a 2007–2010 outbreak in the Netherlands affected over 4,000 people, largely due to urbanized goat farming.
3. Risk Factors
Certain populations face higher risks:
- Occupational Groups: Farmers, veterinarians, and slaughterhouse workers are most vulnerable due to frequent animal contact.
- Geographic Proximity: Living within 3–5 miles of infected farms increases exposure risk.
- Immunocompromised Individuals: Those with weakened immune systems, heart valve defects, or pregnancy are prone to severe or chronic Q fever.
- Urban Exposure: Sporadic cases occur in urban areas from contact with infected pets or occasional farm visits.
Symptoms of Q Fever
Q fever presents in two forms: acute and chronic, with symptoms varying widely. Many infections are asymptomatic, with up to 50% of cases showing no symptoms.
Understanding Jaundice: Causes, Symptoms, Prevention, and Treatment
1. Acute Q Fever
Acute Q fever develops 2–3 weeks after exposure and resembles flu-like illness. Symptoms include:
- High fever (up to 41°C) and chills
- Severe headaches
- Muscle aches and joint pain
- Nausea, vomiting, or diarrhea
- Chest pain or shortness of breath (if pneumonia develops)
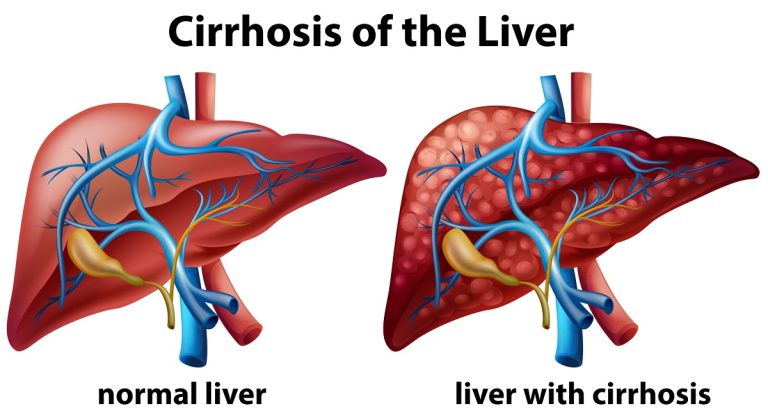
- Hepatitis or liver inflammation
- Fatigue
Most cases resolve within weeks without treatment, but some require antibiotics.
2. Chronic Q Fever
Chronic Q fever, affecting 1–5% of infected individuals, is far more serious and can develop months or years after initial infection. Chronic Q fever has been found to cause damage to the heart and other organs. Common manifestations include:
- Endocarditis: Inflammation of heart valves, the most frequent chronic form, often fatal if untreated.
- Vascular Infections: Affects blood vessels, increasing risk in those with aneurysms or grafts.
- Chronic Fatigue Syndrome (QFS): Prolonged fatigue lasting months or years, as seen in a case reported in 2024.
- Osteomyelitis or Hepatitis: Rare but severe complications affecting bones or liver.
Symptoms include low-grade fever, night sweats, weight loss, and shortness of breath.
3. Q Fever in Pregnancy
Pregnant women are at risk for complications like miscarriage or preterm delivery. The Mayo Clinic advises managing maternal infection post-delivery to avoid risks to the fetus.
Obesity: Causes, Risks, and Weight Management
Diagnosis of Q Fever
Diagnosing Q fever is challenging due to its nonspecific symptoms and delayed antibody response. Key diagnostic methods include:
- Serologic Testing: The indirect fluorescent antibody (IFA) test detects antibodies to C. burnetii phase I and II antigens. Acute infection shows higher phase II IgG titers, while chronic infection shows phase I IgG titers ≥1:1024. Paired samples (taken 3–6 weeks apart) confirm a fourfold rise in titers.
- Polymerase Chain Reaction (PCR): Detects C. burnetii DNA in blood or tissue during the first week of illness, before antibodies appear. PCR sensitivity decreases after doxycycline treatment.
- Clinical History: Recent animal exposure, travel to rural areas, or high-risk occupations guide diagnosis.
Serologic tests are limited in early infection, as antibodies develop 2–3 weeks post-exposure, as noted by the National Institutes of Health (NIH). Chronic cases may require imaging (e.g., echocardiography for endocarditis) or tissue biopsies.
Prevention of Q Fever
Preventing Q fever requires a “One Health” approach, integrating human, animal, and environmental strategies. Reduce your risk of getting Q fever by avoiding contact with animals, especially while animals are giving birth is strongly recommended by the CDC. Key prevention measures include:
1. Occupational and Environmental Controls
- Hygiene Practices: Use protective equipment (masks, gloves) when handling livestock or animal products, especially during birthing.
- Proper Waste Disposal: Safely dispose of birth products and animal waste to minimize aerosolization.
- Pasteurization: Consume only pasteurized milk and dairy products, as C. burnetii can survive in raw milk.
2. Vaccination
A Q fever vaccine (Q-Vax) is available in Australia and has shown over 95% efficacy over five years. However, no vaccine is licensed in the United States or most other countries. High-risk groups (e.g., veterinarians, farmers) in endemic areas should consult healthcare providers about vaccination where available.
3. Public Awareness and Education
Educating at-risk populations about Q fever transmission is critical. Awareness programs and ensuring pasteurization of dairy milk before human consumption would help prevent Q fever zoonosis. Also, community outreach, particularly in rural areas, can reduce misdiagnosis and under-reporting.
Kidney Stones: Treatment, Prevention, Foods to Avoid, and What to Expect
4. Animal Surveillance
Regular testing of livestock for C. burnetii and culling infected animals (as done in the Netherlands outbreak) can curb outbreaks. The European Food Safety Authority (EFSA) suggests, “Preventive vaccination of animals is considered the most effective control measure.”
Treatment of Q Fever
Treatment varies by disease phase and patient condition:
- Acute Q Fever: The CDC recommends doxycycline (100 mg every 12 hours for 14 days) as the first-line treatment. Most patients recover fully, though fluoroquinolones or macrolides may be used for doxycycline-allergic patients.
- Chronic Q Fever: Requires prolonged antibiotic therapy (e.g., doxycycline combined with hydroxychloroquine for 18–24 months) to prevent relapse, particularly in endocarditis cases. The NIH recommends, “Tetracyclines are still considered the mainstay of antibiotic therapy for acute Q fever, whereas antibiotic combinations are necessary for chronic cases.”
- Pregnancy and Pediatrics: Cotrimoxazole is used in pregnant women or children under 8 to avoid doxycycline’s risks.
Post-exposure prophylaxis is not recommended for naturally occurring Q fever, as it’s only effective within 8–12 days of exposure.
Complications and Public Health Impact
Untreated Q fever can lead to severe complications:
- Chronic Q Fever: Endocarditis or vascular infections can be fatal, with mortality rates approaching 100% without treatment.
- Q Fever Fatigue Syndrome (QFS): Affects 20% of acute cases, causing prolonged fatigue and reduced quality of life.
- Economic Burden: Outbreaks, like Australia’s, cost millions annually due to healthcare expenses and lost productivity.
Q fever’s global prevalence is under-reported, with 164–215 annual cases in the U.S. (2016–2018) and 400–600 in Australia (2003–2017), as reported by the CDC. Developing countries, like Pakistan, face higher burdens due to poor surveillance.
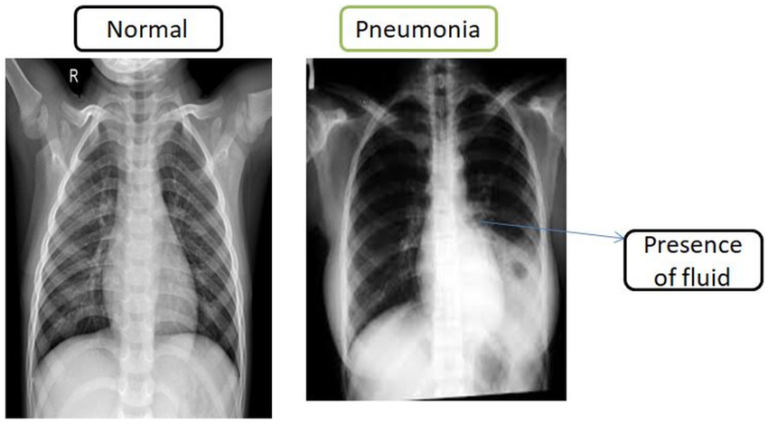
Pneumonia: Symptoms, Treatment, and Recovery Timeline
Addressing the “Forgotten” Status
Q fever’s neglect stems from its asymptomatic nature in animals, nonspecific symptoms in humans, and limited diagnostic access in developing regions. The WHO classifies it among neglected zoonotic diseases prone to misdiagnosis. A “One Health” approach—integrating human, animal, and environmental health—is critical for control. Pathobiological studies including host-pathogen relationships, epidemiology, and genomic information would help understand and identify potential outbreaks.
If you work with animals or live near livestock, it’s important to discuss Q fever risks with your healthcare provider.
Common Causes of Infertility in Men and Women and Treatments