Ovarian cancer, often called the “silent killer,” is a serious disease that affects the ovaries, the reproductive organs responsible for producing eggs and hormones. It’s the fifth leading cause of cancer deaths in women, with about 1 in 78 women developing it in their lifetime, according to the American Cancer Society. Its reputation as a silent disease stems from its subtle symptoms, which often go unnoticed until the cancer has progressed. Early detection significantly improves survival rates, yet only 20% of cases are found before the cancer spreads.
This comprehensive guide explores the following:
✔ What ovarian cancer is and its types
✔ Early warning signs and symptoms
✔ Diagnosis and staging
✔ Treatment options (surgery, chemotherapy, immunotherapy)
✔ Prevention and early detection strategies
By understanding ovarian cancer, you can take proactive steps to protect your health.
What Is Ovarian Cancer?
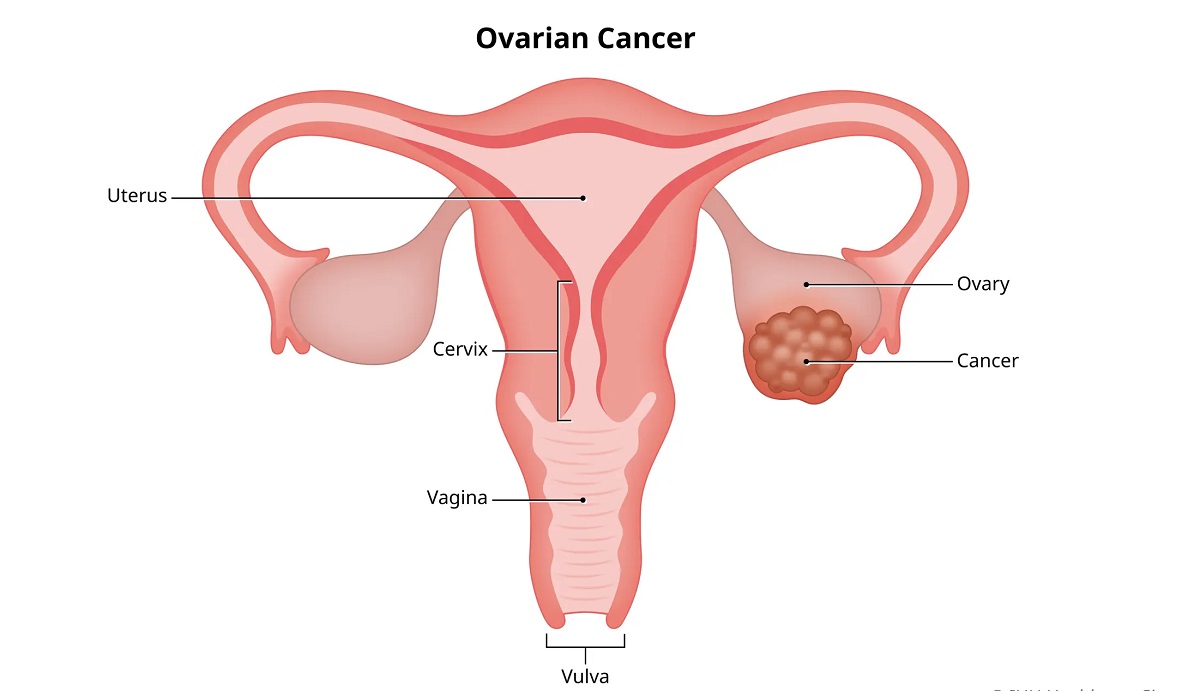
Ovarian cancer originates in the ovaries, fallopian tubes, or peritoneum (the tissue lining the abdominal cavity). It occurs when abnormal cells grow uncontrollably, forming tumors that can spread to other parts of the body. There are several types of ovarian cancer, including:
- Epithelial Ovarian Cancer: The most common type, accounting for 85-90% of cases, originating in the surface layer of the ovaries.
- Germ Cell Tumors: Rare, arising from the cells that produce eggs, often affecting younger women.
- Stromal Tumors: Originate in the hormone-producing cells of the ovary, also rare.
- Primary Peritoneal Cancer: Develops in the peritoneum and behaves similarly to epithelial ovarian cancer.
According to the National Cancer Institute, ovarian cancer includes cancers of the ovaries, fallopian tubes, and primary peritoneal cavity, which are closely related in terms of biology and treatment.
Recommended: Ovarian Cancer and Genetics: What You Should Know
Why Early Detection Is Critical
Ovarian cancer is often diagnosed at an advanced stage (III or IV) because its early symptoms are vague and mimic other conditions. Early detection significantly improves outcomes: the 5-year survival rate for stage I ovarian cancer is around 90%, compared to less than 30% for stage IV. Unfortunately, only about 20% of cases are diagnosed at an early stage, making awareness of symptoms and risk factors essential.
The Ovarian Cancer Research Alliance (OCRA) emphasizes, “Early detection of ovarian cancer saves lives. Knowing the symptoms and your risk factors can make a significant difference.”
Symptoms of Ovarian Cancer
Ovarian cancer symptoms are often subtle and may be mistaken for gastrointestinal or menstrual issues. Common symptoms include:
- Abdominal Bloating or Swelling: A feeling of fullness or pressure in the pelvis or abdomen.
- Pelvic or Abdominal Pain: Persistent discomfort or cramping.
- Feeling Full Quickly or Difficulty Eating: Loss of appetite or early satiety.
- Urinary Symptoms: Frequent or urgent need to urinate, even without a urinary tract infection.
- Fatigue: Unexplained tiredness or low energy.
- Back Pain: Particularly in the lower back, unrelated to physical activity.
- Changes in Bowel Habits: Constipation or diarrhea that persists.
- Menstrual Irregularities: Changes in menstrual cycles or postmenopausal bleeding.
- Unexplained Weight Loss or Gain: Especially if accompanied by other symptoms.
Symptoms of ovarian cancer are not specific and may be caused by other conditions, but if they persist for more than a few weeks, consult a doctor.
Understanding Cancer: Symptoms, Staging, and Survival Tips
When to See a Doctor
Seek medical attention if you experience persistent symptoms (lasting more than 2–3 weeks), especially if you have a family history of ovarian or breast cancer. Early consultation with a gynecologist or oncologist can lead to timely testing and diagnosis.
Risk Factors for Ovarian Cancer
While ovarian cancer can affect anyone, certain factors increase the likelihood:
- Age: Most cases occur in women over 50, with peak incidence between 55 and 64.
- Family History: A history of ovarian, breast, or colorectal cancer in close relatives increases risk, particularly if linked to BRCA1 or BRCA2 gene mutations.
- Genetic Mutations: Inherited mutations in BRCA1, BRCA2, or Lynch syndrome-related genes (e.g., MLH1, MSH2) elevate risk.
- Personal Cancer History: A history of breast, uterine, or colorectal cancer increases the likelihood.
- Reproductive History: Never having been pregnant, early menstruation, or late menopause may increase risk.
- Hormone Replacement Therapy (HRT): Long-term use, especially without progesterone, may elevate risk.
- Obesity: A higher body mass index (BMI) is associated with increased risk.
- Endometriosis: This condition may slightly increase the risk of certain ovarian cancer types.
Women with BRCA1 or BRCA2 mutations have a 10–30% chance of developing ovarian cancer, compared to a 1.3% risk in the general population, as noted by MD Anderson.
Diagnosis of Ovarian Cancer
Diagnosing ovarian cancer involves a combination of medical history, physical exams, imaging, and laboratory tests. Key diagnostic steps include:
- Pelvic Exam: A doctor checks for abnormalities in the ovaries or uterus, though small tumors may not be detectable.
- Imaging Tests:
- Transvaginal Ultrasound: Uses sound waves to visualize the ovaries and detect masses.
- CT or MRI Scans: Provide detailed images to assess tumor size and spread.
- Blood Tests:
- CA-125: Elevated levels may indicate ovarian cancer, though it’s not specific and can be elevated in benign conditions.
- HE4 or OVA1: Additional markers to assess cancer risk.
- Biopsy: A tissue sample, usually obtained during surgery, confirms the diagnosis.
- Genetic Testing: Recommended for those with a family history to identify BRCA or other mutations.
There is no standard screening test for ovarian cancer, so doctors rely on symptoms, risk factors, and diagnostic tests to identify it.
Recommended: How to Prevent HIV: Safe Practices and Testing
Challenges in Screening
Unlike breast or cervical cancer, ovarian cancer lacks a reliable screening test for the general population. Routine pelvic exams or CA-125 tests are not recommended for low-risk women due to high false-positive rates. High-risk individuals (e.g., those with BRCA mutations) may undergo regular ultrasounds and CA-125 tests, but these are not foolproof.
Treatment Options for Ovarian Cancer
Treatment for ovarian cancer typically involves a combination of surgery, chemotherapy, and sometimes targeted therapies or radiation. The approach depends on the cancer’s stage, type, and the patient’s overall health.
1. Surgery
Surgery is often the first step for diagnosis and treatment, aiming to remove as much of the tumor as possible (debulking).
- Total Hysterectomy and Bilateral Salpingo-Oophorectomy: Removal of the uterus, ovaries, and fallopian tubes.
- Omentectomy: Removal of the omentum (fatty tissue in the abdomen) if cancer has spread.
- Lymph Node Dissection: Removal of nearby lymph nodes to check for cancer spread.
- Cytoreductive Surgery: For advanced stages, removes visible tumors in the abdomen.
The Mayo Clinic believes surgery is usually the first treatment for ovarian cancer, and the goal is to remove all visible cancer.
2. Chemotherapy
Chemotherapy uses drugs to kill cancer cells or stop their growth, often administered after surgery to target remaining cancer cells.
- Common Drugs: Carboplatin and paclitaxel are standard for epithelial ovarian cancer.
- Administration: Intravenous (IV) or intraperitoneal (directly into the abdominal cavity) for advanced cases.
- Side Effects: Nausea, fatigue, hair loss, and increased infection risk.
For recurrent or resistant cancers, additional drugs like gemcitabine or liposomal doxorubicin may be used.
3. Targeted Therapies
Targeted therapies focus on specific molecular pathways involved in cancer growth.
- PARP Inhibitors: Drugs like olaparib (Lynparza) or niraparib (Zejula) are effective for BRCA-mutated cancers, blocking cancer cells’ ability to repair DNA.
- Anti-Angiogenesis Drugs: Bevacizumab (Avastin) inhibits blood vessel growth to starve tumors.
Recommended: HIV/AIDS Myths, Facts, and How to Stay Protected
4. Radiation Therapy
Radiation is rarely used for ovarian cancer but may be considered for localized recurrence or symptom relief.
5. Clinical Trials
Clinical trials offer access to cutting-edge treatments, such as immunotherapy or novel targeted therapies. It can also provide access to innovative treatments not yet widely available.
6. Supportive Care
Palliative care addresses symptoms like pain, nausea, or fatigue, improving quality of life. It’s often used alongside active treatment, especially for advanced stages.
Recovery and Follow-Up Care
Recovery from ovarian cancer treatment varies based on the stage and treatment intensity:
- Post-Surgery: Hospital stays typically last 3–7 days, with full recovery taking 6–8 weeks. Avoid heavy lifting and follow wound care instructions.
- Post-Chemotherapy: Side effects may linger for weeks or months. Regular blood tests monitor CA-125 levels and overall health.
- Long-Term Monitoring: Follow-up visits every 3–6 months include physical exams, imaging, and CA-125 tests to detect recurrence.
Regular follow-up after treatment is crucial to monitor for recurrence, as ovarian cancer often comes back.
Importance of Early Detection
Early detection is the cornerstone of better outcomes for ovarian cancer. Strategies to improve early detection include:
- Know Your Body: Track persistent symptoms and report them promptly.
- Genetic Testing: Women with a family history of ovarian or breast cancer should consider BRCA testing.
- High-Risk Screening: Those with genetic mutations or strong family history may benefit from regular ultrasounds and CA-125 tests.
- Advocacy: Discuss concerns with a gynecologist, especially if symptoms persist.
Awareness of symptoms and prompt action can lead to earlier diagnosis, when treatment is most effective.
Prostate Cancer: Warning Signs, Diagnosis, and Treatment
Lifestyle and Prevention Strategies
While ovarian cancer cannot always be prevented, certain measures may reduce risk:
- Oral Contraceptives: Long-term use (5+ years) reduces ovarian cancer risk by up to 50%.
- Pregnancy and Breastfeeding: Both are associated with lower risk.
- Surgical Options: For high-risk women (e.g., BRCA mutation carriers), prophylactic removal of ovaries and fallopian tubes (salpingo-oophorectomy) significantly reduces risk.
- Healthy Lifestyle: Maintain a healthy weight, eat a balanced diet rich in fruits and vegetables, and exercise regularly.
Complications and Long-Term Effects
Ovarian cancer and its treatments can lead to complications:
- Recurrence: Common in advanced stages, requiring additional treatment.
- Menopause Symptoms: Surgical removal of ovaries induces early menopause, causing hot flashes, vaginal dryness, or bone loss.
- Emotional Impact: Anxiety, depression, or body image issues are common. Support groups or counseling can help.
- Fertility Challenges: Treatments may affect fertility, so discuss preservation options (e.g., egg freezing) before starting.
Living with Ovarian Cancer
Living with ovarian cancer involves managing physical and emotional challenges:
- Support Systems: Connect with organizations like OCRA or support groups for emotional and practical support.
- Nutrition: A dietitian can help manage treatment side effects and maintain strength.
- Mental Health: Therapy or mindfulness practices can address the emotional toll of diagnosis and treatment.
Conclusion
Ovarian cancer is a formidable disease, but early detection and advances in treatment offer hope for better outcomes. By recognizing symptoms, understanding risk factors, and seeking prompt medical care, women can improve their chances of early diagnosis and effective treatment. From surgery and chemotherapy to targeted therapies and clinical trials, treatment options are evolving, providing personalized approaches to care. Stay proactive about your health and always consult with specialists for guidance. Early detection is key—know the symptoms, trust your instincts, and act swiftly to protect your health.