Prostate cancer is the second most common cancer in men worldwide, with about 1 in 8 men diagnosed during their lifetime. While many cases grow slowly and require minimal treatment, aggressive forms can be life-threatening if not caught early. Early detection and advances in treatment have improved outcomes significantly, with a 5-year survival rate of nearly 98% for localized cases.
Understanding the warning signs, diagnostic process, and treatment options is crucial for early detection and effective management.
What Is Prostate Cancer?
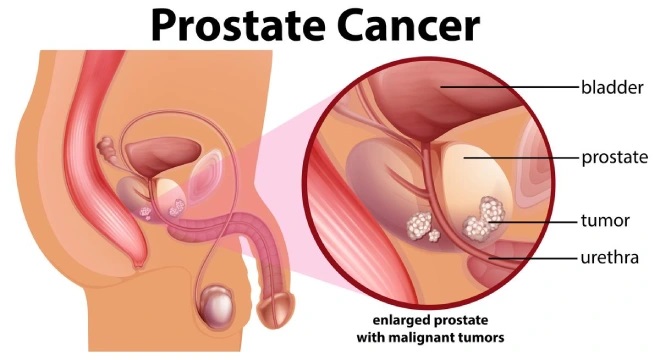
Prostate cancer develops in the prostate gland, a small walnut-shaped organ in men that produces seminal fluid, which nourishes and transports sperm. The cancer occurs when cells in the prostate grow uncontrollably, forming tumors that may remain localized or, in advanced cases, spread to other parts of the body, such as bones or lymph nodes. Most prostate cancers are adenocarcinomas, originating in gland cells, though rare types like sarcomas or small cell carcinomas exist.
The disease often progresses slowly, and many men live with it for years without symptoms, especially in early stages.
Warning Signs of Prostate Cancer
Prostate cancer often develops without noticeable symptoms in its early stages, making screening critical for early detection. When symptoms do appear, they may include:
- Urinary Problems: Difficulty starting or stopping urination, weak urine flow, frequent urination (especially at night), or a feeling of incomplete bladder emptying.
- Blood in Urine or Semen: Hematuria or hematospermia may indicate prostate issues.
- Pelvic or Lower Back Pain: Persistent pain in the pelvis, lower back, hips, or thighs, often in advanced stages.
- Erectile Dysfunction: Difficulty achieving or maintaining an erection.
- Unexplained Weight Loss or Fatigue: Common in advanced cancer that has spread.
Many of these symptoms can be caused by noncancerous conditions like benign prostatic hyperplasia (BPH), so it’s important to see a doctor for an accurate diagnosis.
Recommended: Ovarian Cancer and Genetics: What You Should Know
When to See a Doctor
Men should seek medical attention if they experience persistent urinary symptoms, blood in urine or semen, or unexplained pain. Men over 50, or those with risk factors like a family history of prostate cancer, should discuss screening with their doctor, even without symptoms.
Risk Factors for Prostate Cancer
While the exact cause of prostate cancer is unknown, several factors increase the likelihood of developing it:
- Age: Risk increases significantly after age 50, with most cases diagnosed in men over 65.
- Family History: A father, brother, or son with prostate cancer doubles or triples the risk. Genetic mutations like BRCA1 or BRCA2 also increase risk.
- Race/Ethnicity: African American men have a higher risk and are more likely to develop aggressive forms of the disease.
- Diet and Lifestyle: Diets high in red meat or high-fat dairy and low in fruits and vegetables may increase risk. Obesity is also a factor.
- Genetic Mutations: Inherited mutations in genes like BRCA1, BRCA2, or Lynch syndrome-related genes elevate risk.
- Geographic Location: Prostate cancer is more common in North America and Europe, possibly due to screening practices or environmental factors.
The Prostate Cancer Foundation notes, “African American men have a 60% higher risk of developing prostate cancer and are twice as likely to die from it compared to Caucasian men.”
Understanding Cancer: Symptoms, Staging, and Survival Tips
Diagnosis of Prostate Cancer
Diagnosing prostate cancer involves a combination of screening, clinical evaluation, and diagnostic tests. Early detection is key, as localized prostate cancer is highly treatable.
Screening Tests
Screening aims to detect prostate cancer before symptoms appear, particularly in men at average or high risk.
- Prostate-Specific Antigen (PSA) Test: A blood test measures PSA levels, a protein produced by the prostate. Elevated PSA may indicate cancer, though noncancerous conditions like BPH or prostatitis can also raise levels.
- Digital Rectal Exam (DRE): A doctor physically examines the prostate through the rectum to feel for abnormalities like lumps or hardness.
Diagnostic Tests
If screening suggests cancer, further tests confirm the diagnosis:
- Prostate Biopsy: A needle removes small tissue samples from the prostate, analyzed for cancer cells. Often guided by ultrasound or MRI.
- Multiparametric MRI: Provides detailed images of the prostate to guide biopsies and assess cancer extent.
- Gleason Score: After a biopsy, pathologists assign a Gleason score (6–10) to grade the aggressiveness of cancer cells.
- Imaging Tests: CT, MRI, or bone scans check for cancer spread in advanced cases.
- PSMA PET Scan: A newer imaging technique using prostate-specific membrane antigen to detect cancer spread with high accuracy.
Understanding Ovarian Cancer: Symptoms and Treatment – Early Detection is Key
Staging
Staging determines the cancer’s extent:
- Stage I–II: Cancer is confined to the prostate (localized).
- Stage III: Cancer has spread to nearby tissues.
- Stage IV: Cancer has metastasized to lymph nodes, bones, or other organs.
Treatment Options for Prostate Cancer
Prostate Cancer treatment depends on the cancer’s stage, grade (Gleason score), PSA levels, and the patient’s age, health, and preferences. Options range from monitoring to aggressive interventions.
1. Active Surveillance or Watchful Waiting
For low-risk, slow-growing cancers (e.g., Gleason 6), monitoring may be recommended to avoid unnecessary treatment.
- Active Surveillance: Regular PSA tests, DREs, and biopsies to monitor cancer progression. This is suitable for younger men with low-risk prostate cancer to avoid or delay treatment side effects.
- Watchful Waiting: Less intensive monitoring for older men or those with significant health issues, focusing on symptom management.
2. Surgery
- Radical Prostatectomy: Removes the entire prostate gland and surrounding tissues. Can be open, laparoscopic, or robotic-assisted.
- Side Effects: Urinary incontinence and erectile dysfunction are common but often improve over time.
3. Radiation Therapy
- External Beam Radiation Therapy (EBRT): Delivers high-energy beams to the prostate, often used for localized or locally advanced cancer.
- Brachytherapy: Implants radioactive seeds in the prostate to deliver targeted radiation.
- Side Effects: Bowel or bladder irritation, erectile dysfunction.
4. Hormone Therapy (Androgen Deprivation Therapy, ADT)
Hormone therapy reduces testosterone levels, which fuel prostate cancer growth.
- Medications: LHRH agonists (e.g., leuprolide), anti-androgens (e.g., bicalutamide).
- Surgical Castration: Removal of the testicles (orchiectomy) to lower testosterone.
- Side Effects: Hot flashes, loss of libido, osteoporosis.
5. Chemotherapy
Used for advanced or metastatic prostate cancer, drugs like docetaxel or cabazitaxel target rapidly dividing cancer cells. Often combined with hormone therapy.
6. Targeted Therapies and Immunotherapy
- PARP Inhibitors: Drugs like olaparib (Lynparza) are effective for men with BRCA mutations and advanced cancer.
- Immunotherapy: Sipuleucel-T (Provenge) stimulates the immune system to attack prostate cancer cells, used for metastatic cases.
- PSMA-Targeted Therapy: Lutetium-177 PSMA therapy delivers radiation directly to cancer cells expressing PSMA.
The Prostate Cancer Foundation notes, “Targeted therapies like PARP inhibitors have revolutionized treatment for men with specific genetic mutations”.
7. Clinical Trials
Clinical trials offer access to novel treatments, such as new immunotherapies or combination therapies.
8. Supportive Care
Palliative care manages symptoms like pain or fatigue, improving quality of life, especially in advanced stages.
Recommended: How to Prevent HIV: Safe Practices and Testing
Prevention and Risk Reduction
While prostate cancer cannot be fully prevented, certain measures may lower risk:
- Healthy Diet: Eat a diet rich in fruits, vegetables, and whole grains, and limit red meat and high-fat dairy. Lycopene (found in tomatoes) and cruciferous vegetables (e.g., broccoli) may offer protective benefits.
- Exercise: Regular physical activity helps maintain a healthy weight and may reduce risk.
- Screening: Discuss PSA screening with your doctor, especially if you have risk factors like family history or African American ancestry.
- Avoid Smoking: Smoking may increase the risk of aggressive prostate cancer.
- Genetic Counseling: Men with a family history of prostate, breast, or ovarian cancer should consider genetic testing for BRCA or other mutations.
A healthy lifestyle, including a balanced diet and regular exercise, may help lower prostate cancer risk, though more research is needed.
Recovery and Follow-Up Care
Recovery depends on the treatment approach:
- Post-Surgery: Recovery from prostatectomy takes 4–8 weeks, with potential for temporary incontinence or erectile dysfunction.
- Post-Radiation: Side effects like fatigue or urinary issues may persist for weeks but often improve.
- Advanced Cancer: Ongoing treatment (e.g., hormone therapy) requires regular monitoring for side effects and cancer progression.
Follow-up care includes:
- PSA Monitoring: Regular PSA tests to detect recurrence or treatment response.
- Imaging: CT, MRI, or PSMA PET scans for advanced cases.
- Lifestyle Adjustments: Continue a healthy diet and exercise to support recovery and overall health.
After treatment, regular follow-up is essential to monitor for recurrence and manage side effects.
Recommended: HIV/AIDS Myths, Facts, and How to Stay Protected
Complications and Long-Term Effects
Prostate cancer and its treatments can lead to complications:
- Urinary Incontinence: Common after surgery or radiation, often improving with pelvic floor exercises.
- Erectile Dysfunction: May result from surgery, radiation, or hormone therapy, with treatments like medications or implants available.
- Bone Health: Hormone therapy increases the risk of osteoporosis; calcium, vitamin D, and exercise help.
- Emotional Impact: Anxiety or depression may arise; support groups or counseling can help.
- Metastasis: Advanced cancer may spread to bones, causing pain or fractures.
Living with Prostate Cancer
Living with prostate cancer involves managing physical and emotional challenges:
- Support Networks: Organizations like the Prostate Cancer Foundation offer resources, support groups, and educational materials.
- Sexual Health: Discuss erectile dysfunction treatments with your doctor, such as sildenafil or penile rehabilitation.
- Mental Health: Therapy or mindfulness practices can address the emotional toll of diagnosis and treatment.
- Partner Communication: Open discussions with partners about treatment side effects can strengthen relationships.
Skin Cancer: Warning Signs, Diagnosis, and Prevention
Conclusion
Prostate cancer is a common but often manageable disease, especially when detected early. By recognizing warning signs, understanding risk factors, and pursuing timely diagnosis, men can improve their outcomes. From active surveillance to advanced therapies like PARP inhibitors, treatment options are diverse and increasingly personalized. Preventive measures, including a healthy lifestyle and screening discussions, are crucial for at-risk individuals. Stay proactive by consulting a healthcare provider, especially if you have a family history or symptoms. Knowledge, early detection, and informed decisions are key to managing prostate cancer effectively.