What Are Autoimmune Disorders?
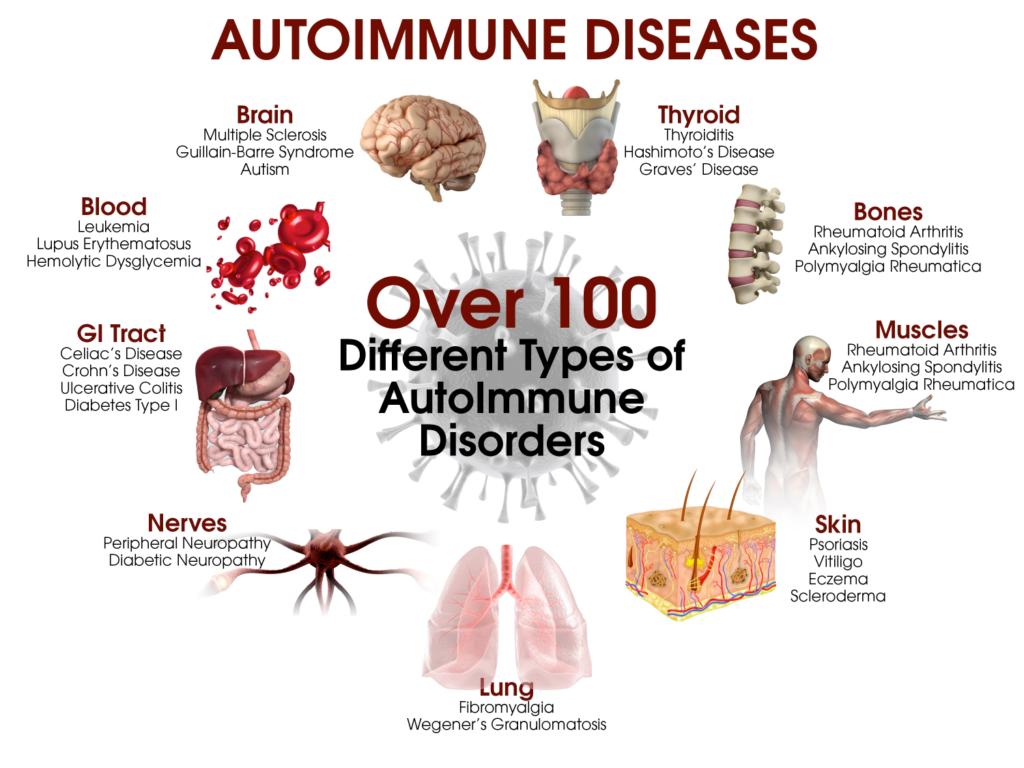
Autoimmune disorders are a group of conditions where the immune system mistakenly attacks the body’s own tissues, leading to a wide range of symptoms and health challenges. With over 80 known autoimmune diseases, including rheumatoid arthritis, lupus, and type 1 diabetes, these conditions affect millions worldwide.
Autoimmune disorders occur when the immune system, which normally protects the body from infections and foreign invaders, turns against healthy cells and tissues. According to the National Institute of Allergy and Infectious Diseases (NIAID), this misdirected immune response can target specific organs (e.g., the thyroid in Hashimoto’s thyroiditis) or multiple systems (e.g., in systemic lupus erythematosus).
Autoimmune disorders are often chronic, with symptoms that can flare up and subside over time. They can affect virtually any part of the body, including joints, skin, muscles, and organs, leading to diverse symptoms and complications.
Yeast Infections (Candidiasis): Causes, Symptoms, and Treatment
Key Characteristics of Autoimmune Disorders
- Immune System Dysfunction: The immune system produces autoantibodies or immune cells that attack healthy tissues.
- Chronic Nature: Most autoimmune disorders are lifelong, though symptoms can be managed.
- Diverse Presentation: Symptoms vary widely depending on the specific condition and affected organs.
- Higher Prevalence in Women: The American Autoimmune Related Diseases Association (AARDA) notes that women are disproportionately affected, making up about 75% of cases.
Common Types of Autoimmune Disorders
There are over 80 autoimmune disorders, but some of the most prevalent include:
- Rheumatoid Arthritis (RA): Attacks joints, causing pain and swelling.
- Systemic Lupus Erythematosus (SLE): Affects multiple organs, including skin, kidneys, and heart.
- Type 1 Diabetes: Destroys insulin-producing cells in the pancreas.
- Multiple Sclerosis (MS): Damages the nervous system, affecting movement and sensation.
- Hashimoto’s Thyroiditis: Targets the thyroid, leading to hypothyroidism.
- Psoriasis: Causes rapid skin cell turnover, resulting in scaly patches.
Causes of Autoimmune Disorders
The exact cause of autoimmune disorders is not fully understood, but a combination of genetic, environmental, and hormonal factors is believed to contribute. The NIAID outlines key factors to include:
1. Genetic Predisposition
Genetics play a significant role in autoimmune disease risk. Certain genes, such as those in the HLA (human leukocyte antigen) family, are associated with increased susceptibility. The Arthritis Foundation notes that a family history of autoimmune disorders raises the likelihood of developing one, though specific conditions may vary.
Understanding Bacterial Infections: Prevention and Treatment
2. Environmental Triggers
Environmental factors can trigger or exacerbate autoimmune disorders in genetically predisposed individuals. Some potential triggers are:
- Infections (e.g., Epstein-Barr virus)
- Exposure to toxins or chemicals
- Smoking
- Stressful life events
3. Hormonal Influences
Hormonal changes, particularly in women, may contribute to autoimmune disorders. For instance, fluctuations in estrogen, such as during pregnancy or menopause, can influence immune activity, hence, the higher prevalence in women.
4. Other Risk Factors
- Age: Many autoimmune disorders develop in young adulthood or middle age.
- Obesity: Excess weight can increase inflammation, worsening symptoms.
- Diet: Poor nutrition may contribute to immune dysregulation.
Recognizing the Signs of Autoimmune Disorders
Symptoms of autoimmune disorders vary widely depending on the condition and affected organs, but some common signs can indicate an autoimmune issue.
Common Symptoms
- Fatigue: Persistent tiredness, even with adequate rest.
- Joint Pain and Stiffness: Common in RA and lupus, often worse in the morning.
- Skin Changes: Rashes (e.g., lupus butterfly rash) or scaly patches (psoriasis).
- Fever: Low-grade fever or feeling feverish without infection.
- Swelling and Redness: Inflammation in joints or other tissues.
- Digestive Issues: Abdominal pain, diarrhea, or weight loss in conditions like Crohn’s disease.
- Neurological Symptoms: Numbness, tingling, or muscle weakness in MS.
Systemic Symptoms
Some autoimmune disorders affect multiple systems, leading to symptoms like:
- Hair loss (e.g., alopecia areata)
- Sensitivity to cold or heat (e.g., thyroid disorders)
- Recurrent infections or slow healing due to immune dysfunction
The Lupus Foundation of America emphasizes that symptoms may come and go, making early recognition challenging. Persistent or recurring symptoms warrant medical evaluation.
Diabetes Type 1 vs Type 2: What’s the Difference?
Diagnosing Autoimmune Disorders
Diagnosing autoimmune disorders can be complex due to overlapping symptoms and the need to rule out other conditions. The National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) outlines the diagnostic process below:
Diagnostic Tools
- Medical History and Physical Exam: Doctors assess symptoms, family history, and physical signs like joint swelling or rashes.
- Blood Tests:
- Autoantibody Tests: Detect specific antibodies, such as antinuclear antibodies (ANA) for lupus or rheumatoid factor (RF) for RA.
- Inflammation Markers: Elevated erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) indicate inflammation.
- Organ-Specific Tests: Thyroid function tests for Hashimoto’s or blood glucose for type 1 diabetes.
- Imaging: X-rays, MRIs, or ultrasounds assess organ or joint damage.
- Biopsy: Tissue samples (e.g., skin or kidney) may confirm certain conditions.
Diagnosis often requires a specialist, such as a rheumatologist or endocrinologist, to interpret results and confirm the condition.
Treatment Options for Autoimmune Disorders
Treatment aims to reduce immune activity, manage symptoms, and prevent complications. Plans are tailored to the specific disorder and individual needs. The common approaches are:
1. Medications
- Immunosuppressants: Drugs like methotrexate or azathioprine suppress immune activity.
- Corticosteroids: Prednisone reduces inflammation but is used short-term due to side effects.
- Biologics: Targeted therapies like adalimumab (Humira) or rituximab block specific immune pathways.
- Anti-Inflammatory Drugs: NSAIDs like ibuprofen alleviate pain and swelling.
- Disease-Specific Treatments: Insulin for type 1 diabetes or thyroid hormone replacement for Hashimoto’s.
Understanding Bipolar Disorder: Types, Symptoms, Diagnosis, and Treatments
2. Lifestyle Changes
- Anti-Inflammatory Diet: Foods rich in omega-3s, fruits, and vegetables (e.g., Mediterranean diet) may reduce inflammation.
- Exercise: Low-impact activities like yoga or swimming improve mobility and reduce stress.
- Stress Management: Mindfulness, meditation, or therapy can help manage flares triggered by stress.
- Adequate Sleep: Rest supports immune regulation and overall health.
3. Physical and Occupational Therapy: Therapy can improve joint function, reduce pain, and teach adaptive techniques for daily tasks.
4. Alternative Therapies
Some patients explore complementary approaches like acupuncture or supplements, however, it is advisable to consult a doctor to ensure safety and efficacy.
5. Surgery
In severe cases, surgery (e.g., joint replacement for RA or thyroidectomy for thyroid disorders) may be needed. Surgery is always the last resort only when damage is significant.
Coping with Autoimmune Disorders
Living with an autoimmune disorder requires emotional and physical resilience. The following strategies can help:
- Support Groups: Connecting with others can provide emotional support and practical tips.
- Education: Learn about your condition to advocate for your health.
- Mental Health Care: Therapy or counseling can address anxiety or depression, which are common with chronic illnesses.
- Pacing Activities: Balance activity and rest to avoid overexertion.
Preventing Flares and Complications
While autoimmune disorders cannot be prevented, certain strategies can reduce flares and complications:
- Avoid Triggers: Identify and minimize exposure to triggers like stress or certain foods.
- Regular Checkups: Monitor disease activity and adjust treatments as needed.
- Vaccinations: Stay up-to-date to prevent infections, which can worsen symptoms.
- Healthy Lifestyle: Maintain a balanced diet, exercise regularly, and avoid smoking.
What You Need to Know About Glaucoma and Blindness
The National Multiple Sclerosis Society emphasizes proactive management to maintain quality of life.
When to Seek Medical Help
It is important to seek medical attention if you experience any of the following:
- Persistent fatigue, joint pain, or rashes
- Unexplained fever or weight loss
- Symptoms that interfere with daily life
- Signs of organ involvement (e.g., shortness of breath, chest pain)
Early diagnosis and treatment can prevent irreversible damage.
Conclusion
Autoimmune disorders are complex, chronic conditions that require early recognition, accurate diagnosis, and tailored treatment to manage effectively. By understanding the signs, seeking timely medical care, and adopting lifestyle changes, individuals can improve their quality of life.
If you suspect an autoimmune disorder, consult a healthcare provider, ideally a specialist, to develop a personalized management plan.
Rheumatoid Arthritis: Causes, Symptoms, Prevention, and Treatment
Understanding Gastrointestinal Discomfort and Treatments that Work
Zollinger-Ellison Syndrome: Rare Digestive Disorder – What You Need to Know