Sjögren’s Syndrome: Causes, Symptoms, and Treatment
Sjögren’s Syndrome is a chronic autoimmune disorder that affects millions worldwide, primarily targeting the body’s moisture-producing glands. If you are experiencing persistent dry eyes, dry mouth, or unexplained fatigue, you might be wondering about Sjögren’s Syndrome causes, symptoms, and available treatments. Whether you are newly diagnosed or seeking more knowledge, understanding Sjögren’s Syndrome can empower you to manage it effectively and improve your quality of life.
In this article, we will explore what Sjögren’s Syndrome is, its underlying causes and risk factors, common and less common symptoms, diagnostic methods, treatment options, potential complications, and practical tips for living with the condition. By the end, you will have a thorough grasp of this often underdiagnosed disease and know when to seek professional help.
What is Sjögren’s Syndrome?
Sjögren’s Syndrome, pronounced “SHOW-gren’s,” is an autoimmune disease where the body’s immune system mistakenly attacks its own moisture-producing glands, leading to chronic dryness in various parts of the body. This primarily affects the salivary glands (which produce saliva) and lacrimal glands (which produce tears), but it can extend to other areas like the skin, vagina, and respiratory tract.
Psoriatic Arthritis: Symptoms, Causes, and Treatment Options
There are two main types of Sjögren’s Syndrome:
- Primary Sjögren’s Syndrome: This occurs independently, without association with other autoimmune diseases. It develops on its own and is not triggered by another condition.
- Secondary Sjögren’s Syndrome: This form is linked to another autoimmune disorder, such as rheumatoid arthritis, lupus, or scleroderma. Nearly half of all Sjögren’s cases are secondary, making it common for patients to have overlapping conditions.
According to estimates, Sjögren’s Syndrome affects around 2 million people in the United States alone, though many cases go undiagnosed due to its subtle onset. It predominantly impacts women, who make up over 90% of cases, and typically emerges between the ages of 45 and 55. The condition is named after Henrik Sjögren, a Swedish ophthalmologist who first described it in the 1930s.
Sjögren’s Syndrome is classified as a systemic autoimmune disease because it can affect multiple organs beyond just the glands. Over time, the inflammation caused by the immune system’s attack reduces the glands’ ability to secrete fluids, leading to the hallmark dryness symptoms.
While there’s no cure, early detection and management can significantly alleviate discomfort and prevent complications.
Causes and Risk Factors of Sjögren’s Syndrome
The exact cause of Sjögren’s Syndrome remains unknown, but research points to a combination of genetic, environmental, and hormonal factors. As an autoimmune disorder, it involves the immune system erroneously targeting healthy tissues, specifically the exocrine glands responsible for moisture production.
Key Causes:
- Genetic Predisposition: Certain genes increase susceptibility. For instance, variants in genes related to immunity, such as those in the major histocompatibility complex (MHC), have been linked to the disease. A genome-wide association study highlighted correlations with the HLA-DQB1 haplotype, suggesting that genetic factors promote abnormal immune responses when combined with triggers.
- Environmental Triggers: Infections, particularly viral ones like Epstein-Barr virus (EBV), hepatitis C, or HIV, may act as catalysts in genetically susceptible individuals. Exposure to solvents, inorganic chemicals, or even bacterial infections could also initiate the autoimmune response.
- Hormonal Influences: The high prevalence in women, especially around menopause, suggests estrogen or other hormones play a role in modulating the immune system.
Rheumatoid Arthritis: Causes, Symptoms, Prevention, and Treatment
Risk Factors:
Several factors heighten the likelihood of developing Sjögren’s Syndrome:
- Age: Most diagnoses occur after age 40, with a peak in the 40s and 50s, notes Johns Hopkins Medicine.
- Sex: Women are 10 times more likely to be affected than men.
- Family History: Having a biological relative with Sjögren’s or another autoimmune disease increases risk.
- Other Autoimmune Conditions: People with rheumatoid arthritis, lupus, or scleroderma are at higher risk, as Sjögren’s often co-occurs with these.
The pathophysiology involves focal lymphocytic sialadenitis (FLS), where lymphocyte-rich cells infiltrate glandular tissue, leading to damage and reduced function. Overexpression of proteins like LAMP3, driven by type I interferons, exacerbates epithelial damage and inflammation. This chronic process can extend to other organs, causing widespread effects.
Symptoms of Sjögren’s Syndrome
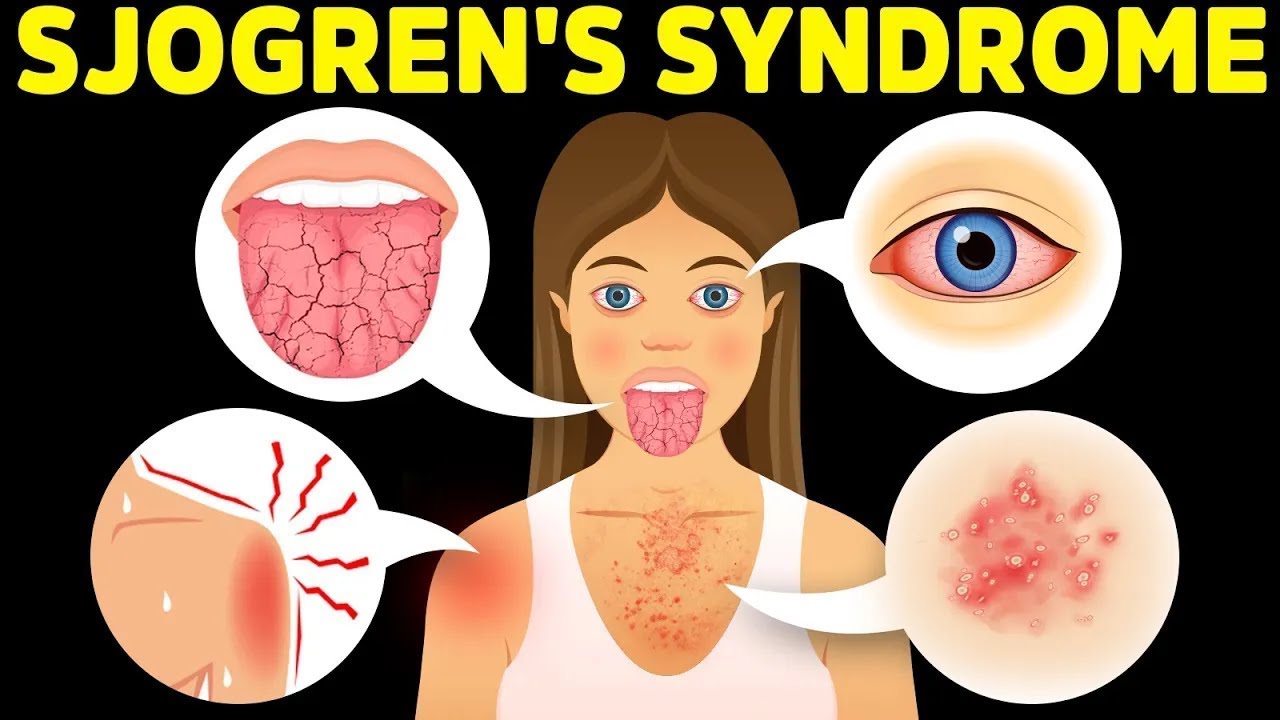
Symptoms of Sjögren’s Syndrome can vary widely, often developing gradually and mimicking other conditions, which delays diagnosis. The hallmark signs are dryness in the eyes and mouth, but the disease can affect the entire body.
Common Symptoms:
- Dry Eyes (Xerophthalmia): Eyes may burn, itch, feel gritty like sand, or become sensitive to light. This can lead to blurred vision or corneal damage.
- Dry Mouth (Xerostomia): The mouth feels cotton-like or chalky, making swallowing, speaking, or tasting difficult. It increases the risk of cavities and oral infections like thrush.
- Fatigue: Persistent tiredness that interferes with daily activities is reported by many patients.
- Joint Pain and Swelling: Arthritis-like symptoms, including stiffness and inflammation, affect up to 50% of cases.
Osteoarthritis: Causes, Symptoms, Prevention, and Treatment
Less Common Symptoms:
- Swollen salivary glands, particularly behind the jaw.
- Dry skin, nasal passages, or vagina.
- Persistent dry cough or shortness of breath.
- Skin rashes, muscle aches, or numbness/tingling in extremities.
- Acid reflux, poor concentration (“brain fog”), or headaches.
Symptoms can flare up and subside, with some individuals experiencing debilitating pain that impacts work and relationships. Extra glandular manifestations, such as lung or kidney involvement, occur in about half of patients, according to NCBI.
How is Sjögren’s Syndrome Diagnosed?
Diagnosing Sjögren’s Syndrome is complex because symptoms overlap with other conditions like medication side effects or fibromyalgia. A rheumatologist typically leads the process, using a combination of clinical evaluation, tests, and criteria from the American College of Rheumatology (ACR)/European League Against Rheumatism (EULAR).
Diagnostic Methods:
- Medical History and Physical Exam: Doctors assess symptoms like dry eyes/mouth and check for gland swelling or dryness signs.
- Blood Tests: These detect autoantibodies (e.g., anti-SSA/Ro, anti-SSB/La), rheumatoid factor, inflammation markers, and organ function.
- Eye Tests: The Schirmer tear test measures tear production (≤5 mm/5 min is abnormal). Slit lamp exams or dye tests reveal surface damage.
- Salivary Tests: Salivary flow rate or scintigraphy assesses saliva production.
- Biopsy: A lip biopsy checks for lymphocytic infiltration in salivary glands, with a focus score ≥1 indicating the disease.
A score of ≥4 on the ACR/EULAR criteria confirms diagnosis, excluding conditions like hepatitis C or sarcoidosis. Early diagnosis is crucial to prevent complications.
Treatment Options for Sjögren’s Syndrome
There’s no cure for Sjögren’s Syndrome, but treatments focus on symptom relief, inflammation reduction, and complication prevention. Management is tailored, often involving a team of specialists like ophthalmologists, dentists, and rheumatologists.
Autoimmune Disorders: Recognizing the Signs, Diagnosis, and Treatment
Medications:
- For Dry Eyes: Prescription eyedrops like cyclosporine (Restasis) or lifitegrast (Xiidra) reduce inflammation, as noted by Cleveland Clinic. Artificial tears provide immediate relief.
- For Dry Mouth: Saliva stimulants like pilocarpine (Salagen) or cevimeline (Evoxac) boost production, says the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). Antifungals treat oral infections.
- Systemic Treatments: Hydroxychloroquine (Plaquenil) or methotrexate for joint pain and inflammation. Corticosteroids or DMARDs for severe cases. According to Arthritis Foundation
- Pain Relief: NSAIDs for joint discomfort; immunosuppressants for organ involvement.
Procedures and Surgeries:
- Punctal Occlusion: Tiny plugs seal tear ducts to retain moisture in the eyes.
- Minor Surgeries: For severe cases, options like gland biopsies or interventions for complications.
Lifestyle and Home Remedies:
- Increase humidity with humidifiers; sip water frequently; use sugar-free gum to stimulate saliva.
- Avoid irritants like smoke, alcohol, or acidic foods. Apply moisturizers for dry skin and use vaginal lubricants.
- Regular dental checkups and fluoride treatments prevent cavities.
Alternative approaches, like acupuncture, may help some, but evidence is limited. For pregnant women with high risk, hydroxychloroquine minimizes complications like congenital heart block.
Understanding Scleroderma: What Causes Skin Tightening and Treatment Options
Complications and Prognosis
Untreated Sjögren’s Syndrome can lead to complications like dental cavities, yeast infections, vision problems, or organ damage (e.g., lungs, kidneys, liver). There’s a small increased risk of lymphoma, particularly non-Hodgkin type.
Prognosis is generally good with management; symptoms often become less intense over time as patients adapt. Life expectancy isn’t typically shortened, but monitoring for flares and complications is essential.
Living with Sjögren’s Syndrome: Tips and Support
Living with Sjögren’s Syndrome requires proactive self-care. Track symptoms in a journal to identify triggers like stress or diet.
Daily tips:
- Hydration: Drink plenty of water; use nasal saline sprays.
- Eye Care: Wear sunglasses outdoors; avoid dry environments.
- Oral Health: Brush/floss regularly; use antimicrobial rinses.
- Diet and Exercise: Eat anti-inflammatory foods; stay active to combat fatigue.
- Work Accommodations: Request flexible hours if needed.
Understanding Hypertension: Causes, Symptoms, and Management
Regular checkups with healthcare providers ensure timely adjustments to treatment plans.
Sjögren’s Syndrome is a manageable condition with the right approach to causes, symptoms, and treatment. If you suspect you have it—such as ongoing dryness or fatigue—consult a doctor promptly for evaluation. Early intervention can prevent complications and enhance your well-being.