Addison’s disease, also known as primary adrenal insufficiency, is a rare but potentially life-threatening disorder where the adrenal glands fail to produce sufficient hormones such as cortisol and, often, aldosterone. Affecting approximately 1 in 100,000 people, according to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), this disorder requires lifelong management and can significantly impact health if untreated. Early diagnosis and proper treatment are crucial to prevent severe complications, including Addisonian crisis, a medical emergency.
In this in-depth guide, we’ll explore:
✅ What causes Addison’s disease?
✅ Early and advanced symptoms
✅ How doctors diagnose adrenal insufficiency
✅ Hormone replacement therapy options
✅ Lifestyle management and emergency care
✅ Latest research and future treatments
This comprehensive guide explores the symptoms, diagnosis, and hormone therapy options for Addison’s disease, empowering readers with evidence-based insights to understand and manage this condition.
Bleeding Disorders: What You Need to Know About Hemophilia
What Is Addison’s Disease?
Addison’s disease occurs when the adrenal glands, located above the kidneys, cannot produce enough cortisol (a stress hormone) and aldosterone (a hormone regulating sodium and potassium balance). Cortisol helps the body respond to stress, maintain blood sugar, and regulate metabolism, while aldosterone controls blood pressure and electrolyte balance. As the Mayo Clinic notes, “Addison’s disease is treatable, but without proper management, it can lead to life-threatening complications.”
The condition can result from autoimmune disorders, infections, or genetic factors and affects both men and women equally, often appearing in adults aged 30–50.
What Are the Adrenal Glands?
The adrenal glands, located on top of each kidney, produce essential hormones:
- Cortisol – Helps regulate metabolism, blood pressure, and stress response.
- Aldosterone – Controls sodium and potassium balance, affecting blood pressure.
- Androgens (e.g., DHEA) – Influence sex drive and muscle strength.
When these glands are damaged, hormone levels drop, leading to Addison’s disease.
Causes of Addison’s Disease
1. Autoimmune Destruction (Most Common Cause – ~80% of Cases)
The immune system mistakenly attacks the adrenal cortex. This is often linked to:
- Autoimmune polyendocrine syndromes (APS-1 & APS-2)
- Hashimoto’s thyroiditis or type 1 diabetes
“Autoimmune Addison’s disease is the most common cause in developed countries.”
– National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
2. Infections
- Tuberculosis (TB) – A leading cause in developing countries.
- HIV/AIDS-related infections (e.g., CMV, fungal infections)
3. Genetic Disorders
- Adrenoleukodystrophy (ALD) – A rare X-linked metabolic disorder.
- Familial glucocorticoid deficiency
4. Other Causes
- Bleeding into adrenal glands (Waterhouse-Friderichsen syndrome)
- Surgical removal of adrenal glands
- Cancer metastasis
Acne: Causes, Symptoms, and Treatments
Symptoms of Addison’s Disease
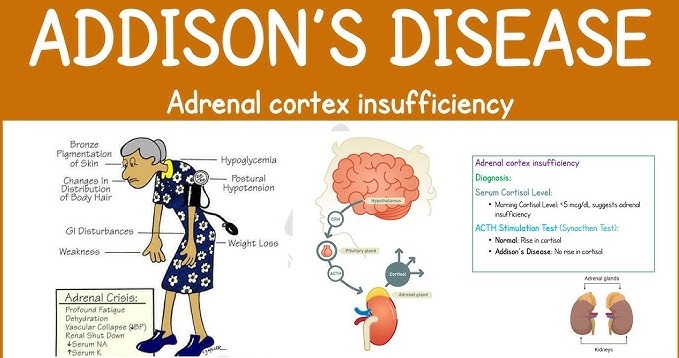
Symptoms of Addison’s disease develop gradually and may be mistaken for other conditions, making early recognition challenging. Common symptoms, as outlined by the Cleveland Clinic, include:
Early Signs (Often Overlooked)
- Chronic Fatigue: Persistent tiredness or weakness that doesn’t improve with rest.
- Weight Loss: Unexplained weight loss due to loss of appetite or nausea.
- Salt Cravings: A strong desire for salty foods caused by low aldosterone levels.
- Muscle or Joint Pain: General aches or weakness.
- Gastrointestinal Issues: Nausea, vomiting, diarrhea, or abdominal pain.
- Low Blood Sugar: Particularly in children, leading to shakiness or confusion.
- Nausea, vomiting, or diarrhea
Advanced Symptoms
- Hyperpigmentation: Darkening of the skin, especially in creases, scars, or areas like the elbows, knees, lips or gums due to excess ACTH stimulating melanin.
- Low Blood Pressure (hypotension): Dizziness or fainting due to aldosterone deficiency.
- Mood Changes: Irritability, depression, or difficulty concentrating.
Addisonian Crisis (A Medical Emergency)
In severe cases, an acute adrenal crisis (Addisonian crisis – a sudden, life-threatening condition) can occur, triggered by severe infection, sudden steroid withdrawal, trauma or surgery. Symptoms include severe dehydration, severe abdominal, back, or leg pain, extreme weakness, low blood pressure, confusion, and loss of consciousness. This is a medical emergency requiring immediate treatment. The National Organization for Rare Disorders (NORD) emphasizes, “An adrenal crisis can be life-threatening if not treated promptly.” While Mayo Clinic notes“An Addisonian crisis requires immediate hydrocortisone injection and IV fluids.”
How is Addison’s Disease Diagnosed?
Diagnosing Addison’s disease involves a combination of clinical evaluation, blood tests, and imaging. According to Johns Hopkins Medicine, “Early diagnosis is critical to prevent complications and improve quality of life.”
Diagnostic Process
- Medical History and Physical Exam: A doctor assesses symptoms, family history, and signs like hyperpigmentation or low blood pressure.
- Blood Tests:
- Morning Cortisol Levels: Low cortisol levels suggest adrenal insufficiency.
- ACTH Stimulation Test: Measures the adrenal glands’ response to adrenocorticotropic hormone (ACTH). Lack of cortisol increase indicates Addison’s disease.
- Electrolyte Levels: Low sodium and high potassium levels point to aldosterone deficiency.
- ACTH Levels: High ACTH with low cortisol suggests primary adrenal insufficiency.
- Imaging: CT or MRI scans of the adrenal glands may identify structural abnormalities or infections like tuberculosis.
- Antibody Tests: To detect autoimmune causes, which account for 70–90% of cases in developed countries.
Additional Tests
- Renin and aldosterone levels (low aldosterone confirms Addison’s)
- DHEA-S test (low levels may indicate adrenal failure)
“The ACTH stimulation test is the gold standard for diagnosing Addison’s disease.”
– Johns Hopkins Medicine
If you suspect Addison’s disease, consult an endocrinologist. The Endocrine Society offers resources to find a specialist: Endocrine Society Find an Endocrinologist.
Hormone Replacement Therapy for Addison’s Disease
Addison’s disease is a lifelong condition, but hormone replacement therapy can effectively manage symptoms and restore normal function. Treatment focuses on replacing deficient hormones and preventing adrenal crises.
1. Cortisol Replacement (Glucocorticoids)
- Hydrocortisone: The most common medication, taken 2–3 times daily to mimic the body’s natural cortisol rhythm. Dosages vary based on individual needs.
- Prednisone or Dexamethasone: Alternatives for some patients, taken less frequently due to longer-lasting effects.
- Dosing Adjustments: During stress (e.g., illness, surgery), patients may need higher doses, known as “stress dosing,” to prevent an adrenal crisis.
2. Aldosterone Replacement
- Fludrocortisone (Florinef): Replaces aldosterone to regulate sodium and potassium levels, helping maintain blood pressure and hydration. Typically taken once daily.
3. Androgen Replacement (Optional for Some Patients)
- DHEA supplements – May improve energy, mood, and libido in women.
4. Emergency Precautions
Patients carry a medical alert bracelet and an emergency injection kit (e.g., hydrocortisone) for adrenal crises. The NIDDK advises, “Patients with Addison’s disease should be educated on how to manage their condition during emergencies.”
4. Monitoring and Follow-Up
Regular check-ups with an endocrinologist ensure proper dosing and monitor for side effects, such as weight gain or osteoporosis from long-term corticosteroid use.
5. Lifestyle Considerations
- Diet: A balanced diet with adequate sodium intake, especially during hot weather or exercise, supports aldosterone replacement.
- Stress Management: Avoiding extreme stress and learning stress-dosing protocols are crucial.
- Regular Exercise: Improves overall health but should be balanced to avoid overexertion.
The Endocrine Society advices “Patients must never abruptly stop steroids, as this can trigger an adrenal crisis.”
Challenges and Misconceptions
Addison’s disease is often underdiagnosed due to its nonspecific symptoms. Common misconceptions include:
- Myth: Addison’s disease is always caused by autoimmune issues. Fact: While autoimmune causes are common, infections (e.g., tuberculosis) or genetic disorders can also trigger it.
- Myth: Hormone therapy fully cures the condition. Fact: Hormone therapy manages symptoms but requires lifelong adherence and monitoring.
Social media platforms may share unverified remedies or misinformation about adrenal health. Always consult trusted medical sources or professionals for guidance.
Daily Management Tips
✔ Take medications at the same time daily.
✔ Monitor blood pressure and electrolytes.
✔ Stay hydrated and consume enough salt.
✔ Exercise moderately (avoid overexertion).
Emergency Preparedness
- Carry a steroid emergency card/bracelet.
- Keep an emergency hydrocortisone injection kit (e.g., Solu-Cortef).
- Inform family/friends about adrenal crisis symptoms.
When to Seek Immediate Help
If you experience symptoms like persistent fatigue, weight loss, or darkening skin, consult a healthcare provider promptly. For suspected adrenal crises (severe weakness, confusion, or fainting), seek emergency care immediately.
Conclusion
Addison’s disease is a chronic but manageable condition with proper hormone replacement and lifestyle adjustments. Early diagnosis is critical to preventing life-threatening complications. By recognizing symptoms early, seeking expert care, and adhering to treatment, individuals can lead healthy, active lives. Consult trusted medical professionals and reliable resources to navigate this condition effectively.