Yeast infections, medically known as candidiasis, are common fungal infections caused by an overgrowth of Candida species, most often Candida albicans. These infections can affect various parts of the body, including the skin, mouth, throat, genitals, and bloodstream, leading to a range of symptoms from mild discomfort to severe complications. According to the Centers for Disease Control and Prevention (CDC), Candida is a normal part of the body’s microbial flora but can cause infections when its growth becomes uncontrolled. Yeast infections are particularly common in women, with about 75% experiencing at least one vaginal yeast infection in their lifetime.
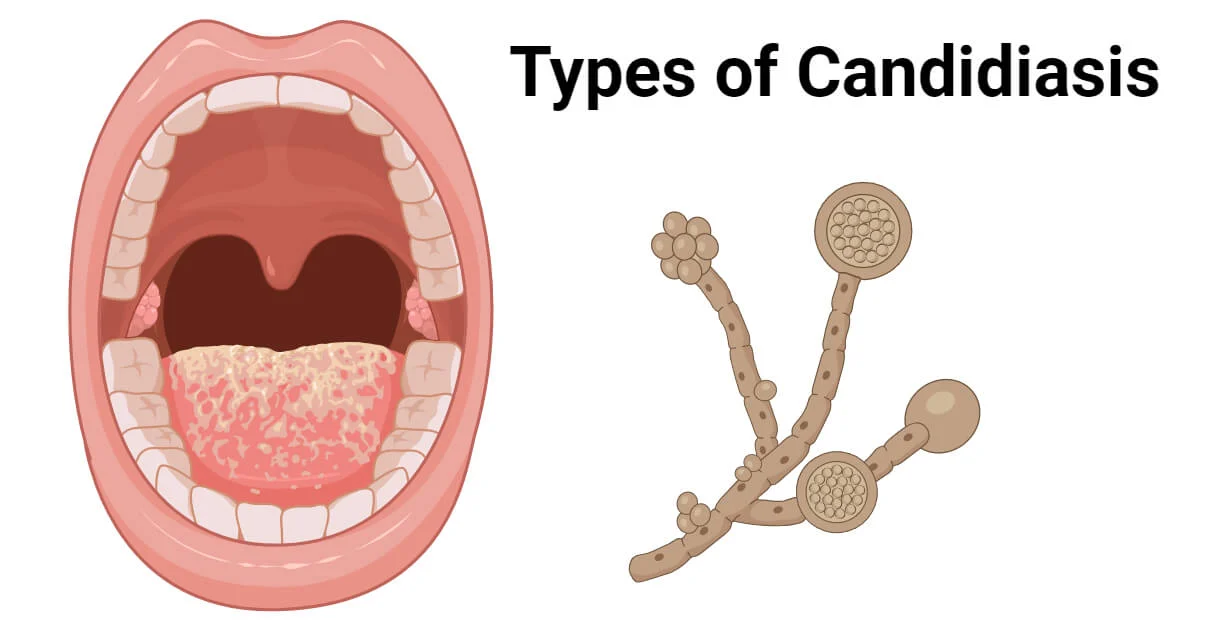
What is Candidiasis?
Candidiasis occurs when Candida fungi, which normally reside in small amounts on the skin, in the mouth, gut, and vagina, multiply excessively, leading to infection. The condition can manifest in various forms, including vaginal candidiasis, oral thrush, cutaneous candidiasis, and invasive candidiasis, depending on the affected area. While most yeast infections are superficial and treatable, severe cases, particularly in immunocompromised individuals, can lead to systemic infections that require urgent medical attention.
Understanding the causes, recognizing symptoms early, and pursuing appropriate treatment are crucial for managing candidiasis and preventing complications.
Common Causes of Infertility in Men and Women and Treatments
Causes of Yeast Infections
Yeast infections result from an imbalance that allows Candida to overgrow. Several factors contribute to this imbalance, including environmental, physiological, and lifestyle triggers. Key causes include:
- Antibiotic Use: Antibiotics can disrupt the balance of bacteria in the body, reducing beneficial bacteria that keep Candida in check. This is a common cause of vaginal yeast infections. “Antibiotics can kill the good bacteria that normally keep yeast in check,” notes the Cleveland Clinic.
- Hormonal Changes: Fluctuations in estrogen levels, such as during pregnancy, menstruation, or while using hormonal contraceptives or hormone replacement therapy, can promote Candida overgrowth, particularly in the vagina.
- Weakened Immune System: Individuals with compromised immunity, such as those with HIV/AIDS, cancer, or undergoing chemotherapy, are at higher risk for candidiasis, including invasive forms. Diabetes, if poorly controlled, also increases susceptibility due to elevated blood sugar levels that feed Candida.
- Moisture and Warmth: Candida thrives in warm, moist environments, making areas like the groin, underarms, or skin folds prone to cutaneous candidiasis, especially in humid climates or with poor hygiene.
- Medications: Corticosteroids and immunosuppressive drugs can weaken the immune system, increasing the risk of yeast infections.
- Diet and Lifestyle: A diet high in sugar or refined carbohydrates can fuel Candida growth. Tight clothing, synthetic fabrics, or prolonged exposure to wet clothing (e.g., swimsuits) can also create favorable conditions for infection.
- Medical Conditions: Conditions like diabetes or obesity increase the risk of candidiasis by altering the body’s microbial balance or creating skin folds where Candida can proliferate.
Symptoms of Yeast Infections
The symptoms of candidiasis vary depending on the affected area. Below are the most common types of yeast infections and their associated symptoms:
- Vaginal Yeast Infections:
- Intense itching or irritation in the vagina or vulva
- Thick, white, “cottage cheese-like” vaginal discharge
- Burning sensation during urination or intercourse
- Redness or swelling of the vulva.
- Oral Thrush:
- White, creamy patches on the tongue, inner cheeks, or throat
- Soreness or difficulty swallowing
- Cracking at the corners of the mouth (angular cheilitis)
- Loss of taste.
- Cutaneous Candidiasis:
- Red, itchy rashes in skin folds (e.g., under breasts, groin, or armpits)
- Pustules or small blisters around the rash
- Scaling or peeling skin.
- Invasive Candidiasis:
- Fever and chills that do not respond to antibiotics
- Organ-specific symptoms if the infection spreads to the bloodstream, heart, or other organs
- Fatigue or weakness in severe cases.
Autoimmune Disorders: Recognizing the Signs, Diagnosis, and Treatment
Symptoms can range from mild to severe, and persistent or recurrent infections may indicate an underlying issue, such as diabetes or immunosuppression, requiring medical evaluation.
Diagnosing Yeast Infections
Accurate diagnosis is essential to distinguish candidiasis from other conditions with similar symptoms, such as bacterial vaginosis or dermatitis. Diagnosis typically involves:
- Medical History and Symptom Review: A healthcare provider will ask about symptoms, recent antibiotic use, medical conditions, or risk factors.
- Physical Examination: For vaginal infections, a pelvic exam may reveal characteristic signs like discharge or redness. Oral thrush is diagnosed by inspecting white patches in the mouth.
- Laboratory Tests:
- Microscopy or Culture: A sample of discharge, skin scrapings, or tissue is examined under a microscope or cultured to confirm Candida presence.
- Blood Tests: For invasive candidiasis, blood cultures or tests for fungal markers are used.
- Endoscopy: In rare cases, to diagnose esophageal candidiasis, an endoscopy may be performed to visualize the throat.
Prompt diagnosis is critical, especially for invasive candidiasis, which can be life-threatening if untreated.
Treatments that Work for Yeast Infections
Treatment for candidiasis depends on the type, severity, and location of the infection. Most yeast infections respond well to antifungal therapies, but underlying conditions must also be addressed to prevent recurrence.
1. Antifungal Medications
- Vaginal Yeast Infections:
- Over-the-Counter (OTC) Treatments: Antifungal creams, ointments, or suppositories (e.g., miconazole, clotrimazole) are effective for uncomplicated infections, typically used for 1–7 days. “Most yeast infections can be treated with over-the-counter antifungal creams or suppositories,” states the Cleveland Clinic.
- Prescription Medications: Oral fluconazole is used for severe or recurrent infections, often as a single dose.
- Oral Thrush:
- Antifungal mouthwashes or lozenges (e.g., nystatin, clotrimazole) are commonly prescribed.
- Oral fluconazole may be used for persistent cases.
- Cutaneous Candidiasis:
- Topical antifungals like ketoconazole or clotrimazole are applied to affected skin areas.
- Invasive Candidiasis:
- Intravenous antifungals like amphotericin B or echinocandins (e.g., caspofungin) are used in hospital settings for systemic infections.
What You Need to Know About Glaucoma and Blindness
2. Addressing Underlying Causes
- Manage Diabetes: Controlling blood sugar levels reduces Candida growth.
- Adjust Medications: Limiting or adjusting antibiotics or corticosteroids can prevent recurrence.
- Immune Support: Treating underlying immune deficiencies, such as HIV, can reduce infection risk.
3. Lifestyle and Home Remedies
- Hygiene Practices: Keep affected areas clean and dry, especially for cutaneous candidiasis. Wear loose, breathable clothing to reduce moisture.
- Dietary Changes: Reducing sugar and refined carbohydrates may help limit Candida growth, though evidence is limited.
- Probiotics: Some studies suggest probiotics may restore beneficial bacteria and reduce vaginal yeast infection recurrence, as noted by Mayo Clinic.
4. Complementary Therapies
- Yogurt with Live Cultures: Applying plain, unsweetened yogurt with live Lactobacillus topically to the vulva (the area around the vaginal opening), inserting it into the vagina, or consuming it as part of your diet may help restore microbial balance.
Note: This is not a substitute for medical treatment, and should therefore be used cautiously and under medical guidance.
5. Managing Recurrent Infections
For individuals with recurrent yeast infections (four or more per year), long-term antifungal therapy (e.g., weekly fluconazole for six months) may be prescribed. Identifying and addressing triggers, such as hormonal imbalances or diabetes, is crucial.
Rheumatoid Arthritis: Causes, Symptoms, Prevention, and Treatment
Preventing Yeast Infections
Preventive measures can reduce the risk of developing or recurring yeast infections:
- Maintain Good Hygiene: Wash regularly and keep skin dry, especially in areas prone to moisture.
- Wear Breathable Clothing: Choose cotton underwear and avoid tight clothing to reduce moisture buildup.
- Limit Antibiotic Use: Use antibiotics only when necessary and discuss probiotics with your doctor to maintain microbial balance.
- Control Blood Sugar: For diabetics, maintaining stable blood sugar levels reduces infection risk.
- Avoid Irritants: Use unscented soaps and avoid douching or feminine hygiene sprays, which can disrupt vaginal flora.
- Regular Check-Ups: Routine medical exams can detect underlying conditions that increase infection risk.
Living with Yeast Infections: Practical Tips
Managing yeast infections, especially recurrent ones, requires proactive steps to maintain health and prevent complications:
- Monitor Symptoms: Keep a symptom diary to identify triggers and discuss with your healthcare provider.
- Seek Prompt Treatment: Treat infections early to prevent worsening or spread, especially in immunocompromised individuals.
- Consult a Specialist: For recurrent or severe infections, a gynecologist, infectious disease specialist, or dermatologist can provide tailored care.
Zollinger-Ellison Syndrome: Rare Digestive Disorder – What You Need to Know
Understanding Gastrointestinal Discomfort and Treatments that Work