Chronic Obstructive Pulmonary Disease (COPD) is a progressive lung condition that affects millions worldwide, making breathing difficult and impacting daily life. Despite its challenges, individuals with COPD can manage symptoms, improve quality of life, and breathe better through proper care, lifestyle changes, and medical interventions. With COPD affecting over 250 million people globally, understanding how to manage this condition is crucial.
What Is COPD?
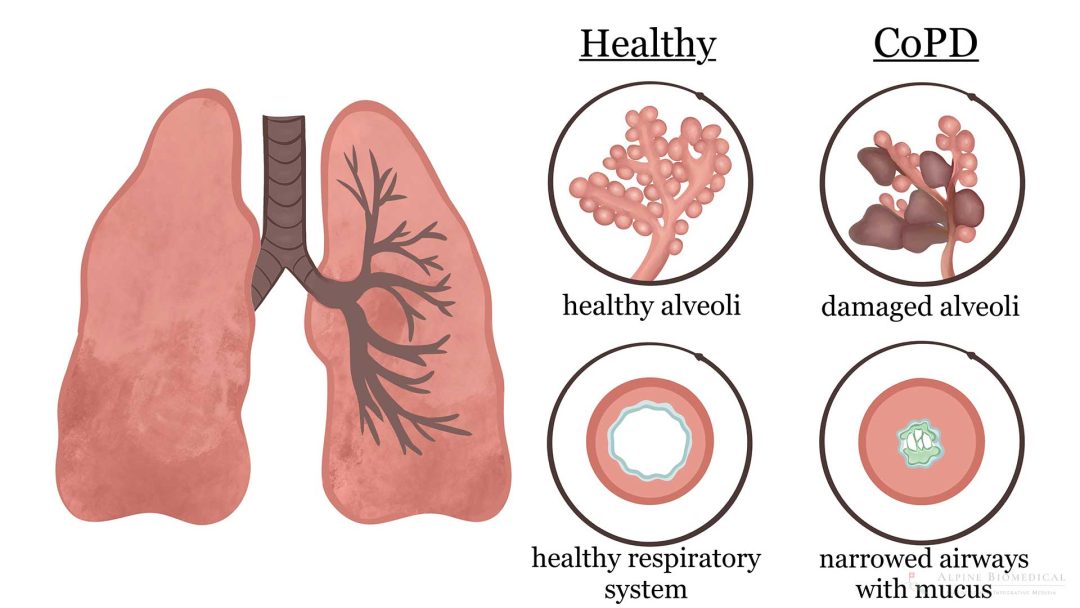
COPD is a group of lung diseases, primarily emphysema and chronic bronchitis, characterized by airflow obstruction that makes breathing difficult. According to the World Health Organization (WHO), COPD affects over 250 million people globally and is the third leading cause of death globally, with 3.23 million deaths in 2019. The condition is often caused by long-term exposure to irritants like cigarette smoke, air pollution, or occupational dusts and chemicals.
- Chronic Bronchitis: Involves a persistent cough with mucus production due to inflamed airways.
- Emphysema: Damages the alveoli (air sacs), reducing oxygen exchange.
See Also: Living with Asthma: Tips for Better Breathing
The American Lung Association notes that COPD is progressive but manageable with proper treatment. Early diagnosis and intervention are key to slowing disease progression and improving quality of life.
Common Symptoms of COPD
COPD symptoms develop gradually and worsen over time, often going unnoticed until significant lung damage occurs. The following are common signs:
- Shortness of Breath: Especially during physical activity, known as dyspnea.
- Chronic Cough: Often with mucus (sputum) production.
- Wheezing: A whistling sound during breathing due to narrowed airways.
- Chest Tightness: A feeling of pressure or constriction in the chest.
- Fatigue: Resulting from reduced oxygen levels and increased breathing effort.
- Frequent Respiratory Infections: Such as colds or pneumonia.
“Many people don’t recognize COPD symptoms until the disease is advanced,” says Dr. MeiLan Han, a pulmonologist quoted by the American Lung Association. Exacerbations, or flare-ups, can worsen symptoms suddenly and require immediate medical attention.
Diagnosis of COPD
Diagnosing COPD involves a combination of medical history, physical exams, and diagnostic tests. While there is no cure, early diagnosis and proper management can significantly improve quality of life. The National Heart, Lung, and Blood Institute (NHLBI) outlines the following key diagnostic tools:
- Spirometry: A lung function test measuring how much air you can exhale and how quickly. It’s the gold standard for confirming COPD, according to NHLBI.
- Chest X-ray or CT Scan: Identifies lung abnormalities like emphysema or other conditions.
- Blood Tests: Measure oxygen and carbon dioxide levels to assess lung function.
- Pulse Oximetry: Checks oxygen saturation in the blood non-invasively.
Recommended: What Triggers Asthma Attacks and How to Avoid Them
Early diagnosis is critical. The CDC reports that many individuals with COPD remain undiagnosed, delaying treatment and worsening outcomes.
Strategies for Breathing Better with COPD
Managing COPD involves a multifaceted approach to reduce symptoms, prevent exacerbations, and enhance overall well-being. Below are evidence-based strategie:
1. Quit Smoking
Smoking is the leading cause of COPD. The American Lung Association emphasizes that quitting smoking slows disease progression significantly. Resources like counseling, nicotine replacement therapy, and medications (e.g., bupropion) can help. “Quitting smoking is the single most important step for COPD patients,” says the NHLBI.
2. Medications
Medications can relieve symptoms and prevent exacerbations. Common options, per the Mayo Clinic, include:
- Bronchodilators: Relax airway muscles (e.g., albuterol, tiotropium).
- Inhaled Corticosteroids: Reduce airway inflammation (e.g., fluticasone).
- Phosphodiesterase-4 Inhibitors: Decrease inflammation in severe COPD (e.g., roflumilast).
- Antibiotics: Treat infections during exacerbations.
Always follow a healthcare provider’s guidance for proper inhaler use and medication adherence.
3. Pulmonary Rehabilitation
Pulmonary rehabilitation is a structured program combining exercise, education, and support. The American Thoracic Society reports that it improves exercise capacity, reduces breathlessness, and enhances quality of life. Programs include:
- Exercise Training: Strengthens respiratory muscles.
- Nutritional Counseling: Addresses weight loss or gain common in COPD.
- Breathing Techniques: Such as pursed-lip breathing to improve oxygen intake.
4. Oxygen Therapy
For individuals with low blood oxygen levels, supplemental oxygen can improve survival and quality of life. The NHLBI notes that oxygen therapy may be used continuously or during activity/sleep, depending on severity.
5. Lifestyle Changes
Adopting healthy habits can significantly improve COPD management:
- Exercise Regularly: Low-impact activities like walking or yoga improve stamina, per the Cleveland Clinic.
- Healthy Diet: A balanced diet rich in fruits, vegetables, and lean proteins supports lung health.
- Avoid Irritants: Minimize exposure to air pollution, dust, and chemical fumes.
- Stay Hydrated: Drinking water thins mucus, making it easier to breathe.
6. Vaccinations
COPD patients are at higher risk for respiratory infections. The CDC recommends:
- Annual flu vaccine.
- Pneumococcal vaccines (PCV13 and PPSV23).
- COVID-19 vaccine and boosters.
7. Manage Exacerbations
Exacerbations can be triggered by infections, air pollution, or stress, to manage this, it’s important to:
- Recognize early signs (increased shortness of breath, change in sputum).
- Follow an action plan provided by your doctor, which may include increased medication or hospitalization.
- Seek immediate care for severe symptoms like chest pain or confusion.
Burns: First Aid Tips Everyone Should Know
Coping with COPD: Emotional and Social Support
COPD can take an emotional toll, leading to anxiety or depression. The American Lung Association recommends:
- Joining support groups to connect with others.
- Seeking counseling or therapy for mental health support.
- Communicating openly with family and friends about your needs.
“Living with COPD requires a team effort,” says pulmonologist Dr. Albert Rizzo of the American Lung Association. Support from healthcare providers, family, and community resources can make a significant difference.
Advanced Treatments and Research
For severe COPD, advanced interventions may be necessary:
- Surgery: Options like lung volume reduction surgery or lung transplant, per the Mayo Clinic.
- Bronchoscopic Interventions: Valves or coils to improve lung function, as studied by the NHLBI.
- Emerging Therapies: Research into biologics and gene therapy is ongoing, with promising trials reported in the Journal of Thoracic Disease.
Prevention and Risk Reduction
While COPD is not fully preventable, reducing risk factors can help. The WHO suggests:
- Avoid smoking and secondhand smoke.
- Reduce exposure to indoor and outdoor air pollutants.
- Use protective gear in high-risk occupations (e.g., mining, construction).
When to Seek Medical Attention
Consult a healthcare provider if you experience:
- Persistent cough, shortness of breath, or wheezing.
- Frequent respiratory infections.
- Symptoms of an exacerbation (e.g., increased mucus, severe dyspnea).
Cirrhosis: Liver Damage Explained and What You Should Do
The American Thoracic Society advises regular check-ups with a pulmonologist to monitor lung function and adjust treatment plans.
Conclusion
Living with COPD presents challenges, but with the right strategies, you can breathe better and lead a fulfilling life. Quitting smoking, adhering to medications, participating in pulmonary rehabilitation, and adopting healthy lifestyle habits are critical steps. Consult your healthcare provider for a personalized plan, and take proactive steps today to breathe easier tomorrow.