Ovarian cancer is a complex and potentially life-threatening disease that affects thousands of women worldwide. It is one of the most lethal gynecological cancers, largely because it’s often diagnosed at an advanced stage. According to the American Cancer Society, approximately 19,680 new cases of ovarian cancer will be diagnosed in the United States in 2025, and about 12,740 women will succumb to the disease. While most cases occur sporadically, 5-10% are linked to inherited genetic mutations. Understanding the genetic risk factors for ovarian cancer can help women make informed decisions about screening, prevention, and treatment.
Understanding Ovarian Cancer
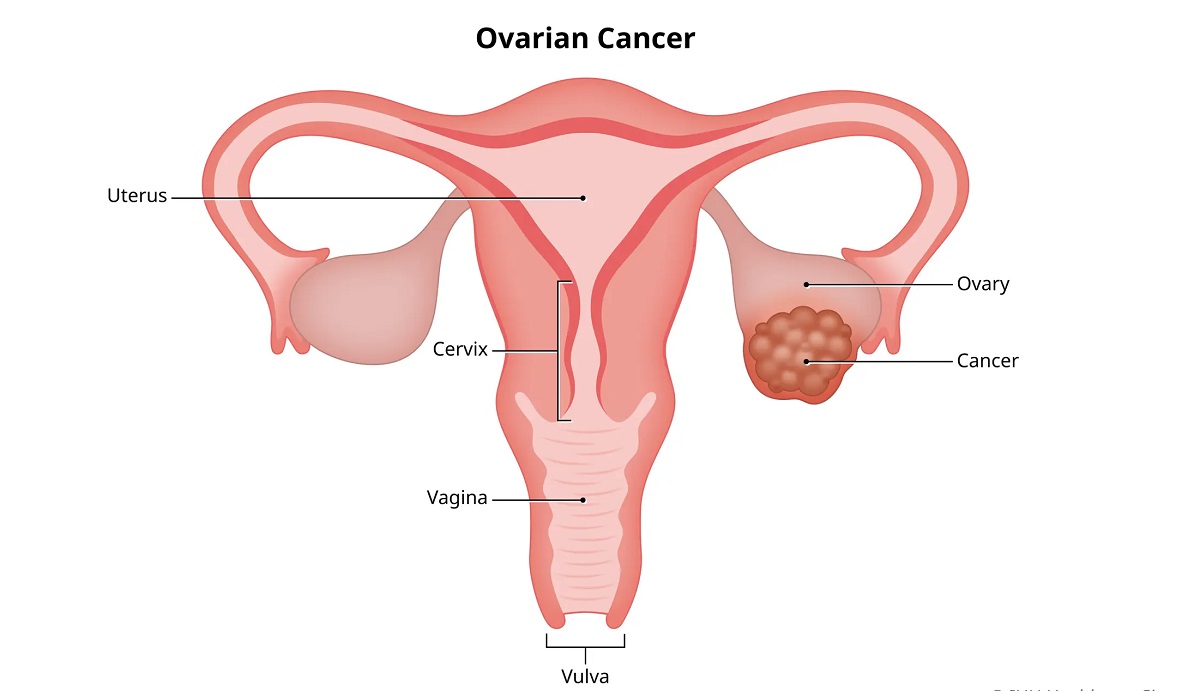
Ovarian cancer originates in the ovaries, fallopian tubes, or peritoneum—the tissue lining the abdominal cavity. It occurs when abnormal cells grow uncontrollably, forming tumors that may spread to other parts of the body. The most common type is epithelial ovarian cancer, which accounts for 85–90% of cases, followed by rare types like germ cell tumors and stromal tumors. A related condition, primary peritoneal cancer, behaves similarly to ovarian cancer and is often treated in the same way.
The National Cancer Institute notes that Ovarian, fallopian tube, and primary peritoneal cancers are closely related and are often grouped together because they share similar characteristics and treatments. While ovarian cancer can develop sporadically (without a clear genetic cause), inherited genetic mutations significantly increase the risk for some individuals.
Understanding Cancer: Symptoms, Staging, and Survival Tips
The Role of Genetics in Ovarian Cancer
Approximately 20–25% of ovarian cancer cases are linked to inherited genetic mutations, making genetics a critical factor in understanding and managing the disease. These mutations are passed down through families and can significantly elevate the risk of developing ovarian cancer, as well as other cancers like breast, pancreatic, or colorectal cancer.
Key Genetic Mutations
- BRCA1 and BRCA2 Mutations
- The BRCA1 and BRCA2 genes (Breast Cancer genes 1 and 2) are tumor suppressor genes that help repair damaged DNA. Mutations in these genes impair DNA repair, increasing the risk of uncontrolled cell growth.
- Women with BRCA1 mutations have a 35–70% lifetime risk of developing ovarian cancer, while those with BRCA2 mutations have a 10–30% risk, compared to a 1.3% risk in the general population.
- BRCA mutations also increase the risk of breast cancer, pancreatic cancer, and, in men, prostate cancer.
- Lynch Syndrome (Hereditary Nonpolyposis Colorectal Cancer, HNPCC)
- Lynch syndrome is caused by mutations in mismatch repair genes (e.g., MLH1, MSH2, MSH6, PMS2). It primarily increases the risk of colorectal and endometrial cancers but also raises ovarian cancer risk by 4–12%.
- Women with Lynch syndrome are also at risk for other cancers, including stomach, pancreatic, and urinary tract cancers.
- Other Genetic Mutations
- Less common mutations associated with ovarian cancer include those in genes like RAD51C, RAD51D, BRIP1, and PALB2. These genes are also involved in DNA repair and are linked to hereditary breast and ovarian cancer syndromes.
- The Ovarian Cancer Research Alliance (OCRA) explains, “While BRCA1 and BRCA2 are the most well-known, other genetic mutations can also contribute to ovarian cancer risk, and research continues to uncover new genetic links.”
Sporadic vs. Hereditary Ovarian Cancer
Most ovarian cancers (75–80%) are sporadic, meaning they occur without an identifiable inherited mutation, often due to random genetic changes acquired over time. In contrast, hereditary ovarian cancer is driven by inherited mutations, typically in BRCA1, BRCA2, or Lynch syndrome-related genes. Identifying whether a case is hereditary or sporadic is crucial for determining risk, screening, and preventive measures for both the patient and their family.
Understanding Ovarian Cancer: Symptoms and Treatment – Early Detection is Key
Who Is at Risk?
While anyone can develop ovarian cancer, certain factors indicate a higher likelihood of a genetic predisposition:
- Family History: A history of ovarian, breast, pancreatic, or colorectal cancer in first-degree relatives (parents, siblings, children) or multiple family members increases the likelihood of a hereditary cancer syndrome.
- Personal Cancer History: A prior diagnosis of breast, endometrial, or colorectal cancer may suggest a genetic link.
- Ashkenazi Jewish Ancestry: Individuals of Ashkenazi Jewish descent have a higher prevalence of BRCA1 and BRCA2 mutations (1 in 40 carry a mutation compared to 1 in 100 in the general population).
- Age at Diagnosis: Ovarian cancer diagnosed before age 50 may indicate a hereditary cause.
- Multiple Cancers: Individuals or families with multiple cancer types (e.g., breast and ovarian) are more likely to have a genetic mutation.
Having a family history of ovarian cancer, breast cancer, or colorectal cancer can increase your risk, especially if the cancers occurred at a young age, as noted by the American Cancer Society.
Genetic Testing for Ovarian Cancer
Genetic testing identifies inherited mutations that increase cancer risk, helping guide prevention and treatment strategies. It’s typically recommended for:
- Women diagnosed with ovarian cancer, especially if diagnosed at a young age or with a family history.
- Individuals with a strong family history of ovarian, breast, or related cancers.
- Those with Ashkenazi Jewish ancestry and a personal or family history of cancer.
- Relatives of someone with a known BRCA or other cancer-related mutation.
How Genetic Testing Works
- Sample Collection: A blood or saliva sample is analyzed for specific gene mutations.
- Panel Testing: Modern tests screen for multiple genes (e.g., BRCA1, BRCA2, Lynch syndrome genes, and others) associated with hereditary cancers.
- Genetic Counseling: Before and after testing, genetic counselors help interpret results, discuss implications, and guide decision-making.
Genetic counseling is recommended before genetic testing to understand the risks, benefits, and limitations of the test.
What Is HIV/AIDS? Symptoms and Transmission
Benefits of Genetic Testing
- Risk Assessment: Identifies individuals at high risk, enabling tailored screening or preventive measures.
- Family Planning: Helps family members understand their risk and consider testing.
- Treatment Guidance: For those with ovarian cancer, knowing mutation status can guide targeted therapies (e.g., PARP inhibitors for BRCA mutations).
- Prevention: High-risk individuals may opt for proactive measures like prophylactic surgery.
Limitations and Considerations
- Incomplete Information: A negative test doesn’t eliminate all risk, as not all genetic mutations are known or tested.
- Emotional Impact: Positive results can cause anxiety or stress about future health.
- Cost and Access: While many insurance plans cover genetic testing for high-risk individuals, costs can be a barrier for some.
- Variant of Uncertain Significance (VUS): Some test results identify mutations with unclear cancer risk, requiring further research.
Symptoms of Ovarian Cancer in the Context of Genetics
Ovarian cancer symptoms are often vague, making early detection challenging, even in genetically predisposed individuals. Common symptoms include:
- Persistent abdominal bloating or swelling
- Pelvic or abdominal pain
- Feeling full quickly or difficulty eating
- Frequent or urgent urination
- Fatigue, back pain, or changes in bowel habits
For women with genetic mutations, symptoms may appear at younger ages or be associated with multiple cancer types. The Mayo Clinic advises, “If you have a family history of ovarian or breast cancer and experience persistent symptoms, consult a doctor promptly.”
Recommended: HIV/AIDS Myths, Facts, and How to Stay Protected
Genetic Mutations and Treatment Options
Genetic information not only informs risk but also shapes treatment for ovarian cancer patients.
1. Surgery
Surgery is the cornerstone of ovarian cancer treatment, regardless of genetic status. Procedures include:
- Hysterectomy and Bilateral Salpingo-Oophorectomy: Removal of the uterus, ovaries, and fallopian tubes.
- Debulking Surgery: Removes as much tumor as possible in advanced cases.
2. Chemotherapy
Chemotherapy (e.g., carboplatin, paclitaxel) is standard for most ovarian cancers, used post-surgery to eliminate residual cancer cells.
3. Targeted Therapies for Genetic Mutations
- PARP Inhibitors: Drugs like olaparib (Lynparza), niraparib (Zejula), and rucaparib (Rubraca) exploit DNA repair weaknesses in BRCA-mutated cancers, significantly improving outcomes. MD Anderson notes, “PARP inhibitors have revolutionized treatment for ovarian cancer patients with BRCA mutations.”
- Other Targeted Therapies: Bevacizumab (Avastin) may be used to inhibit tumor blood vessel growth, though it’s not specific to genetic mutations.
4. Clinical Trials
Patients with hereditary ovarian cancer may benefit from clinical trials testing novel therapies, such as immunotherapy or new targeted drugs. Clinical trials offer access to cutting-edge treatments, especially for those with genetic mutations.
Prostate Cancer: Warning Signs, Diagnosis, and Treatment
Preventive Strategies for High-Risk Individuals
For women with BRCA1, BRCA2, or other high-risk mutations, preventive measures can significantly reduce the likelihood of developing ovarian cancer:
- Prophylactic Surgery
- Risk-Reducing Salpingo-Oophorectomy (RRSO): Removal of the ovaries and fallopian tubes can reduce ovarian cancer risk by up to 96% in BRCA mutation carriers. It’s typically recommended between ages 35–40 for BRCA1 carriers and 40–45 for BRCA2 carriers, after childbearing is complete. RRSO is the most effective way to prevent ovarian cancer in women with BRCA mutations, though it induces early menopause, The National Cancer Institute notes.
- Enhanced Screening
- While no standard screening test exists for ovarian cancer, high-risk women may undergo:
- Transvaginal Ultrasound: To detect ovarian abnormalities.
- CA-125 Blood Tests: To monitor for elevated levels, though not specific to cancer.
- Screening is less effective than surgery but may be used for women not ready for RRSO.
- While no standard screening test exists for ovarian cancer, high-risk women may undergo:
- Chemoprevention
- Oral Contraceptives: Long-term use (5+ years) reduces ovarian cancer risk by up to 50%, even in BRCA mutation carriers, but the decision to use them should weigh other health factors as they may slightly increase breast cancer risk, so discuss with a doctor first.
- Lifestyle Modifications
- Maintain a healthy weight, eat a balanced diet, and exercise regularly to support overall health.
- Avoid long-term use of hormone replacement therapy (HRT) unless medically necessary, as it may increase risk.
Genetic Counseling: A Critical Step
Genetic counseling is essential for anyone considering genetic testing or managing hereditary cancer risk. Counselors provide:
- Risk Assessment: Evaluate family history and personal risk factors.
- Education: Explain the implications of genetic mutations and testing.
- Decision Support: Guide decisions about testing, screening, or preventive surgery.
- Emotional Support: Address the psychological impact of genetic results.
Genetic counseling helps individuals and families understand their cancer risk and make informed choices about their health.
Implications for Family Members
A positive genetic test result has implications for relatives, as mutations are inherited in an autosomal dominant pattern (50% chance of passing to children). Family members may benefit from:
- Cascade Testing: Testing relatives of someone with a known mutation to identify carriers.
- Preventive Measures: High-risk relatives can pursue screening or risk-reducing strategies.
- Support Resources: Organizations like the Ovarian Cancer Research Alliance (OCRA) offer guidance for families navigating hereditary cancer risk.
Knowledge is power—understanding the genetic aspects of ovarian cancer can lead to early detection, personalized treatment, and better outcomes.