Cirrhosis is a chronic liver disease characterized by scarring that impairs the liver’s ability to function effectively. As a progressive condition, it can lead to serious complications if not managed properly. However, with early detection, lifestyle changes, and medical interventions, individuals with cirrhosis can improve their quality of life and slow disease progression.
What Is Cirrhosis?
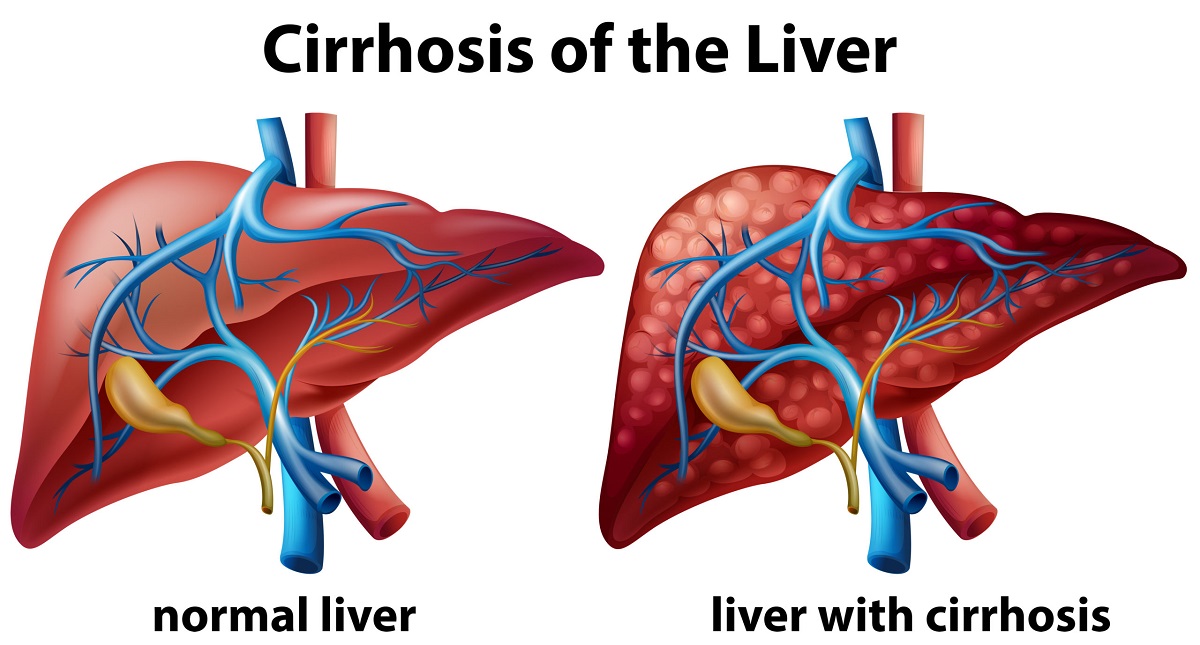
Cirrhosis is the end stage of chronic liver disease, where healthy liver tissue is replaced by scar tissue (fibrosis), severely impairing normal liver function. Over time, this scarring:
- Blocks blood flow through the liver
- Reduces detoxification of harmful substances
- Impairs digestion (due to decreased bile production)
The liver can regenerate to some extent, but severe cirrhosis causes permanent damage.
The liver, a vital organ, detoxifies the blood, produces proteins, and aids digestion. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), cirrhosis develops over years due to ongoing damage, impairing the liver’s ability to perform these tasks. “Cirrhosis is a silent disease in its early stages, often showing no symptoms until significant damage occurs,” notes Dr. Jacqueline O’Leary of the American Liver Foundation.
Chronic Kidney Disease: Early Detection Matters
Cirrhosis can lead to complications like portal hypertension (high blood pressure in the liver’s veins), liver failure, or liver cancer. The World Health Organization (WHO) links cirrhosis to 1.32 million deaths annually, often tied to underlying causes like hepatitis or alcohol-related liver disease.
Causes of Cirrhosis
Cirrhosis results from prolonged liver injury. The common causes are:
- Chronic Alcohol Use: Excessive alcohol consumption over years is a leading cause.
- Viral Hepatitis: Hepatitis B and C cause chronic inflammation and scarring.
- Nonalcoholic Fatty Liver Disease (NAFLD): Linked to obesity and diabetes, NAFLD can progress to nonalcoholic steatohepatitis (NASH) and cirrhosis.
- Autoimmune Hepatitis: The immune system attacks the liver, causing inflammation.
- Genetic Disorders: Conditions like hemochromatosis (iron overload) or Wilson’s disease (copper buildup).
- Biliary Diseases: Primary biliary cholangitis or primary sclerosing cholangitis block bile ducts.
Less common causes include prolonged exposure to toxins, certain medications, or chronic heart failure, per the Cleveland Clinic.
Symptoms of Cirrhosis
Cirrhosis often remains asymptomatic in its early stages, known as compensated cirrhosis. Symptoms appear as the disease progresses to decompensated cirrhosis. The common signs of cirrhosis are:
- Fatigue: Persistent tiredness due to reduced liver function.
- Jaundice: Yellowing of the skin and eyes from bilirubin buildup.
- Abdominal Swelling (Ascites): Fluid accumulation in the abdomen.
- Edema: Swelling in the legs or ankles.
- Easy Bruising or Bleeding: Due to decreased clotting factors.
- Itchy Skin: Caused by bile salt buildup.
- Confusion (Hepatic Encephalopathy): Toxin accumulation affecting brain function.
- Spider Angiomas: Small, spider-like blood vessels on the skin.
“Symptoms like jaundice or ascites signal advanced cirrhosis, requiring urgent medical attention,” warns the American Liver Foundation.
COPD: Breathing Better with Chronic Obstructive Pulmonary Disease
Diagnosis of Cirrhosis
Diagnosing cirrhosis involves a combination of medical history, physical exams, and diagnostic tests.
- Blood Tests: Assess liver function (e.g., ALT, AST, bilirubin levels) and screen for underlying causes like hepatitis.
- Imaging Tests: Ultrasound, CT, or MRI detect liver scarring, size, or nodules.
- Liver Biopsy: A tissue sample confirms cirrhosis and identifies its cause.
- FibroScan: A non-invasive test measures liver stiffness to assess fibrosis.
- Endoscopy: Checks for varices (enlarged veins) due to portal hypertension.
Early diagnosis helps to prevent complications like liver cancer, which develops in 1-5% of cirrhosis patients annually.
Managing Cirrhosis: What You Should Do
While cirrhosis is irreversible, its progression can be slowed, and symptoms managed through lifestyle changes, medical treatments, and monitoring. Below are some tip for managing cirrhosis:
1. Address the Underlying Cause
Treating the root cause can prevent further liver damage:
- Alcohol Cessation: Abstaining from alcohol is critical for alcohol-related cirrhosis.
- Hepatitis Treatment: Antiviral medications for hepatitis B or C can reduce inflammation.
- Weight Management: For NAFLD-related cirrhosis, weight loss through diet and exercise can reverse early damage, says the NIDDK.
2. Medications
Medications manage symptoms and complications:
- Diuretics: Reduce ascites and edema (e.g., furosemide, spironolactone).
- Beta-Blockers: Prevent bleeding from varices (e.g., propranolol).
- Lactulose or Rifaximin: Treat hepatic encephalopathy by reducing toxins.
- Antivirals: Control hepatitis-related inflammation.
Consult a hepatologist for personalized treatment plans.
3. Lifestyle Changes
Healthy habits support liver health:
- Healthy Diet: A low-sodium diet reduces fluid buildup, per the American Liver Foundation. Focus on fruits, vegetables, lean proteins, and whole grains.
- Avoid Alcohol and Toxins: Eliminate alcohol and limit medications like acetaminophen that stress the liver.
- Exercise: Moderate activity improves overall health, but avoid overexertion.
- Vaccinations: Hepatitis A, B, flu, and pneumococcal vaccines prevent infections.
4. Manage Complications
Cirrhosis complications require proactive management:
- Portal Hypertension: Endoscopy or medications prevent variceal bleeding.
- Ascites: Paracentesis (fluid removal) or shunts may be needed.
- Hepatic Encephalopathy: Dietary protein adjustments and medications reduce symptoms.
- Liver Cancer Screening: Regular ultrasounds and alpha-fetoprotein tests detect cancer early.
What Triggers Asthma Attacks and How to Avoid Them
5. Liver Transplantation
For end-stage cirrhosis, a liver transplant may be necessary. The Mayo Clinic notes that transplants are considered when the liver can no longer function adequately (MELD score >15). “A transplant is the only cure for end-stage cirrhosis,” according to the American Liver Foundation
6. Emotional and Social Support
Cirrhosis can impact mental health. The American Liver Foundation recommends:
- Joining support groups to connect with others.
- Seeking counseling for anxiety or depression.
- Communicating with family and healthcare providers for support.
“Living with cirrhosis requires a holistic approach, addressing both physical and emotional needs,” says Dr. O’Leary.
Preventing Cirrhosis
Preventing liver damage reduces cirrhosis risk. The NIDDK advises:
- Limit alcohol to moderate levels (1 drink/day for women, 2 for men).
- Get vaccinated against hepatitis A and B.
- Maintain a healthy weight to prevent NAFLD.
- Avoid sharing needles or unsafe practices that spread hepatitis C.
Burns: First Aid Tips Everyone Should Know
When to Seek Medical Attention
Seek immediate care if you experience:
- Severe abdominal pain or swelling.
- Confusion, disorientation, or severe fatigue.
- Vomiting blood or black, tarry stools.
- Yellowing of the skin or eyes.
Regular check-ups with a hepatologist are essential.
Conclusion
Cirrhosis is a serious condition, but with early intervention, lifestyle changes, and medical care, individuals can manage symptoms and prevent complications. Addressing underlying causes, adopting a healthy lifestyle, and seeking support from trusted resources like the American Liver Foundation, Mayo Clinic, and NIDDK empower those with cirrhosis to live well. Consult a healthcare provider for personalized care, and take proactive steps today to protect your liver and improve your quality of life.