Renal failure also known as kidney failure is a serious and potentially life-threatening health condition that occurs when the kidneys lose their ability to filter waste products and excess fluids from the blood. The kidneys play a crucial role in maintaining the body’s internal balance, including fluid levels, electrolytes, and acid-base status. When they fail to function properly, toxins build up in the body, leading to a range of symptoms and complications that require medical attention.
Understanding Renal Failure
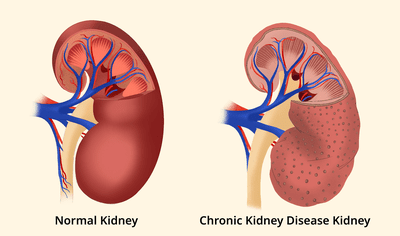
Renal failure happens when the kidneys are no longer able to perform their essential functions at a level needed to sustain life. This can occur suddenly over hours or days (acute) or gradually over months or years (chronic). Renal failure is sometimes referred to as kidney failure or end-stage renal disease (ESRD) especially in its most advanced form, where kidney function drops below 15% of normal, according to National Institute of Diabetes and Digestive and Kidney Diseases, (NIDDK).
The kidneys filter waste products from the blood and regulate electrolytes, fluids, and blood pressure. When they fail, waste products and fluid can accumulate in the blood and tissues, leading to symptoms that range from mild to severe.
Primary Functions of the Kidneys
✔ Filter waste and excess fluid from the blood
✔ Regulate blood pressure
✔ Balance electrolytes (sodium, potassium, calcium)
✔ Stimulate red blood cell production via hormones
✔ Maintain acid-base balance
When these functions are compromised, systemic effects occur which affects the heart, bones, nervous system, and other organs.
Understanding Down Syndrome: Causes, Types, Symptoms, & Treatment Options
Types of Renal Failure
Renal failure is broadly classified into two main types based on how quickly it develops:
- Acute Renal Failure (Acute Kidney Injury — AKI)
Acute renal failure, now more commonly called acute kidney injury (AKI), develops suddenly — often within a few hours or days. It is common in hospitalized patients, especially among those with severe infections, dehydration, or serious illnesses.
According to Mayo Clinic, AKI may be reversible if detected and treated early. It occurs when the kidneys suddenly lose their ability to filter waste from the blood, leading to rapid buildup of toxins and fluid.
- Chronic Renal Failure (Chronic Kidney Disease — CKD)
Chronic renal failure develops gradually over months or years. It’s often caused by long-term conditions such as diabetes or high blood pressure. Chronic kidney disease (CKD) may not cause noticeable symptoms until significant kidney damage has occurred.
When CKD progresses to the point where kidney function is critically low (eGFR < 15), it is called end-stage renal disease (ESRD). At this stage, regular dialysis or a kidney transplant is usually required to sustain life.
Causes of Renal Failure
The causes of renal failure vary depending on whether the condition is acute or chronic.
Common Causes of Acute Renal Failure
According to the Mayo Clinic, acute kidney injury can occur due to three main mechanisms:
- Reduced blood flow to the kidneys (pre-renal)
- Direct damage to the kidneys (intrinsic)
- Obstruction of urine drainage (post-renal)
Examples include:
✔ Severe dehydration or blood loss
✔ Infections or septic shock
✔ Heart failure
✔ Certain medications and toxins
✔ Kidney stones blocking urine flow
✔ Enlarged prostate or tumors blocking urinary tract
✔ Autoimmune conditions like lupus
✔ Muscle breakdown (rhabdomyolysis)
Common Causes of Chronic Renal Failure
Chronic kidney failure usually results from long-term diseases and conditions that slowly damage the kidneys over time, including:
✔ Diabetes (diabetic nephropathy) — damage from high blood sugar
✔ High blood pressure (hypertension) — prolonged high pressure damages kidney vessels
✔ Glomerulonephritis — chronic inflammation of kidney filters
✔ Polycystic kidney disease (PKD) — inherited condition with fluid-filled cysts
✔ Autoimmune diseases such as lupus
✔ Urinary tract obstruction due to stones or tumors
Thrombosis: Symptoms, Causes, Types, and Treatment
Other Risk Factors
Certain individuals are at increased risk of developing renal failure:
- Older age
- Family history of kidney disease
- Long-term use of pain relievers like NSAIDs
- Heart disease
- History of kidney injury
- Certain ethnic groups with higher prevalence of kidney disease
Symptoms of Renal Failure
Symptoms can vary based on whether the condition is acute or chronic, and many symptoms may go unnoticed in early stages.
Symptoms of Acute Renal Failure
Symptoms of AKI may develop quickly and include:
✔ Reduced urine output (less urinating)
✔ Fluid buildup causing swelling in legs, ankles, or face
✔ Tiredness or weakness
✔ Confusion or mental fog
✔ Nausea and vomiting
✔ Loss of appetite
✔ Pain in the side or belly
✔ Irregular heartbeat
✔ Seizures or coma in severe cases
Symptoms of Chronic Renal Failure
Because CKD develops gradually, symptoms often appear late and include:
✔ Fatigue and weakness
✔ Nausea and vomiting
✔ Loss of appetite
✔ Swelling of hands, feet, or face
✔ Shortness of breath
✔ Changes in urination patterns (more or less)
✔ Itchy skin
✔ Trouble sleeping
✔ Muscle cramps
✔ Darkening of the skin
✔ Trouble concentrating or confusion
Some symptoms warrant immediate medical attention, especially sudden changes in urination or rapid swelling paired with other symptoms. Early detection improves outcomes.
Neuralgia: Symptoms, Causes, Types, and Effective Treatments
Stages of Chronic Kidney Disease
Chronic kidney disease progresses through five stages based on the estimated glomerular filtration rate (eGFR), a measure of how well the kidneys filter blood.
| Stage | eGFR (mL/min) | Kidney Function |
| 1 | ≥ 90 | Normal or high function |
| 2 | 60–89 | Mild loss |
| 3a | 45–59 | Mild to moderate loss |
| 3b | 30–44 | Moderate to severe loss |
| 4 | 15–29 | Severe loss |
| 5 | < 15 | Kidney failure (ESRD) |
Complications of Renal Failure
When kidney function declines, complications may develop, including:
- High Blood Pressure: Damaged kidneys cannot regulate blood pressure effectively, which may worsen kidney damage.
- Fluid Retention: Excess fluid can accumulate and lead to swelling or pulmonary edema (fluid in the lungs).
- Electrolyte Imbalances: High potassium (hyperkalemia) can be life-threatening and affect heart rhythm.
- Anemia: Reduced production of erythropoietin (a hormone made by the kidneys) can lead to low red blood cell counts.
- Bone Disease: Kidneys help regulate calcium and vitamin D; dysfunction leads to bone weakness.
- Heart Disease: Kidney failure increases the risk of cardiovascular disease.
Diagnosis of Renal Failure
Diagnosing renal failure involves medical history, physical examination, and several laboratory tests:
Blood Tests
✔ Serum creatinine — high levels indicate poor kidney function
✔ Blood urea nitrogen (BUN) — high levels suggest decreased filtration
✔ GFR estimation — calculates filtration rate to determine stage
Urine Tests
✔ Protein in the urine (proteinuria)
✔ Blood in the urine (hematuria)
Imaging Tests
Ultrasound or CT scan to assess kidney size, structure, or blockages.
Biopsy
In some cases, a kidney biopsy may be needed to diagnose the underlying cause.
Multiple Myeloma: Causes, Symptoms, Diagnosis & Treatment Options
Treatment Options for Renal Failure
- Treat Underlying Causes: For acute kidney failure, identifying and addressing the cause such as dehydration, blood loss, infection, or drug toxicity can often restore kidney function if treated early.
- Lifestyle and Conservative Management: For chronic kidney disease or early kidney failure, treatment focuses on slowing progression:
✔ Blood pressure control
✔ Blood sugar management in diabetes
✔ Dietary changes (limiting salt, protein, potassium)
✔ Avoiding kidney-toxic medications
✔ Maintaining healthy body weight
- Medication Management: Doctors may recommend the following:
- ACE inhibitors or ARBs: helps to lower blood pressure and protect kidneys
- Diuretics: reduce fluid retention
- Statins: control cholesterol
- Erythropoietin-stimulating agents: treat anemia
- Vitamin D and phosphate binders: support bone health
- Dialysis: When the kidneys can no longer remove wastes and fluids effectively, dialysis is required. There are two main types:
- Hemodialysis: A machine filters blood outside the body through an artificial kidney (dialyzer). It is usually done several times per week.
- Peritoneal Dialysis: This method uses the lining of the abdomen to filter blood using a special solution that absorbs waste and fluid, which is then drained.
- Kidney Transplant: A kidney transplant involves placing a healthy kidney from a living or deceased donor into the patient. After transplant, patients must take immunosuppressive medications for life to prevent rejection.
- End-of-Life and Conservative Options: Some individuals may choose conservative management without dialysis or transplant, focusing on maintaining quality of life and managing symptoms with supportive care.
Prevention and Risk Reduction
While not all cases of renal failure are preventable, you can reduce risk by
✔ Managing diabetes and hypertension
✔ Avoiding excessive use of NSAIDs and other nephrotoxic drugs
✔ Staying hydrated
✔ Maintaining a healthy lifestyle
✔ Regular checkups if at risk
Urinary Tract Infections (UTI): Types, Causes, Symptoms, & Effective Treatment
Renal failure is a complex condition that ranges from sudden, acute kidney injury to chronic kidney dysfunction that develops over years. While it can be life-threatening, early diagnosis, careful management, lifestyle changes, and advanced treatments such as dialysis and kidney transplantation have transformed outcomes for millions of people worldwide.